Palliative Care
Session: Palliative Care
429 - Education in Palliative and End-of-Life Care (EPEC)-Pediatrics During the COVID-19 Pandemic: Virtual Versus In-Person Teaching
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 429.4752
Stefan J. Friedrichsdorf, UCSF Benioff Children's Hospital San Francisco, San Francisco, CA, United States; Justin Baker, Stanford University School of Medicine, Half Moon Bay, CA, United States; Davis T. D.. Bullock, University of California, San Francisco, School of Medicine, San Ramon, CA, United States; Joanne Wolfe, Massachusetts General Hospital and Brigham and Women's Hospital, Boston, MA, United States; Stacy S.. Remke, University of Minnesota, St Paul, MN, United States; Ximena Garcia-Quintero, St. Jude Children's Research Hospital, Memphis, TN, United States; Joshua Hauser, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Andrea C. Postier, University of California, San Francisco, School of Medicine, San Francisco, CA, United States

Stefan J. Friedrichsdorf, MD (he/him/his)
Chief, Division of Pediatric Pain, Palliative and Integrative Medicine
UCSF Benioff Children's Hospital San Francisco
San Francisco, California, United States
Presenting Author(s)
Background: EPEC-Pediatrics, funded by the National Cancer Institute in 2010 (R25 CA151000-01), has developed into the most widely disseminated Pediatric Palliative Care (PPC) curriculum worldwide. In response to the COVID-19 pandemic, a virtual training option was introduced in 2020.
Objective: Describe participation of all EPEC-Pediatrics conferences and explore differences between virtual and in-person conference participants regarding knowledge, skills, and attitudes (KSA) of pain and symptom management (PSM) for children with serious illness.
Design/Methods: (1) Abstraction of participant demographics from 31 Train-the-Trainer (TtT) and 10 workshop conferences since 2010. (2) An electronic survey in English and Spanish assessing changes in KSA of PSM was distributed to participants from 19 conferences conducted between 2019 and 2023.
Results: A total of 2,388 clinicians from 126 countries were trained 2012-2024, including 1,421 TtT “Trainers” (Top 7 countries: USA n=394, Canada n=110, India n=103, Australia n=60, Columbia n=43, New Zealand n=41, Uruguay n=38). Twenty-three percent (255/1118) of clinicians who attended between 2019-2023 representing 73 countries responded to the survey. Respondents included 25% fellowship-trained, 83% female and 76% physicians. Most attended in-person (63%) in-person, and 51% attended a TtT conference. Almost all (94%) reported improved prevention and treatment of pain and distressing symptoms of children with serious illness in their institution/region because of EPEC-Pediatrics training. The majority agreed/strongly agreed their KSA in PSM improved (88-92%); however, in-person attendees were more likely to report improved PSM attitudes compared to virtual attendees (x2=10.8, p=0.03). Reported benefits of virtual learning included diverse international interaction, high accessibility (no travel costs, lower fees), and convenience. Cons included a reduced sense of connection, lower physical alertness due to differences of time zones, and routine distractions.
Conclusion(s): While in-person participants reported higher improvement in pain and symptom management attitudes, virtual EPEC-Pediatrics is effective in teaching PPC and expanding global access to this essential training.
Figure 1: 1,421 EPEC-Pediatrics “Trainers" from 95 countries
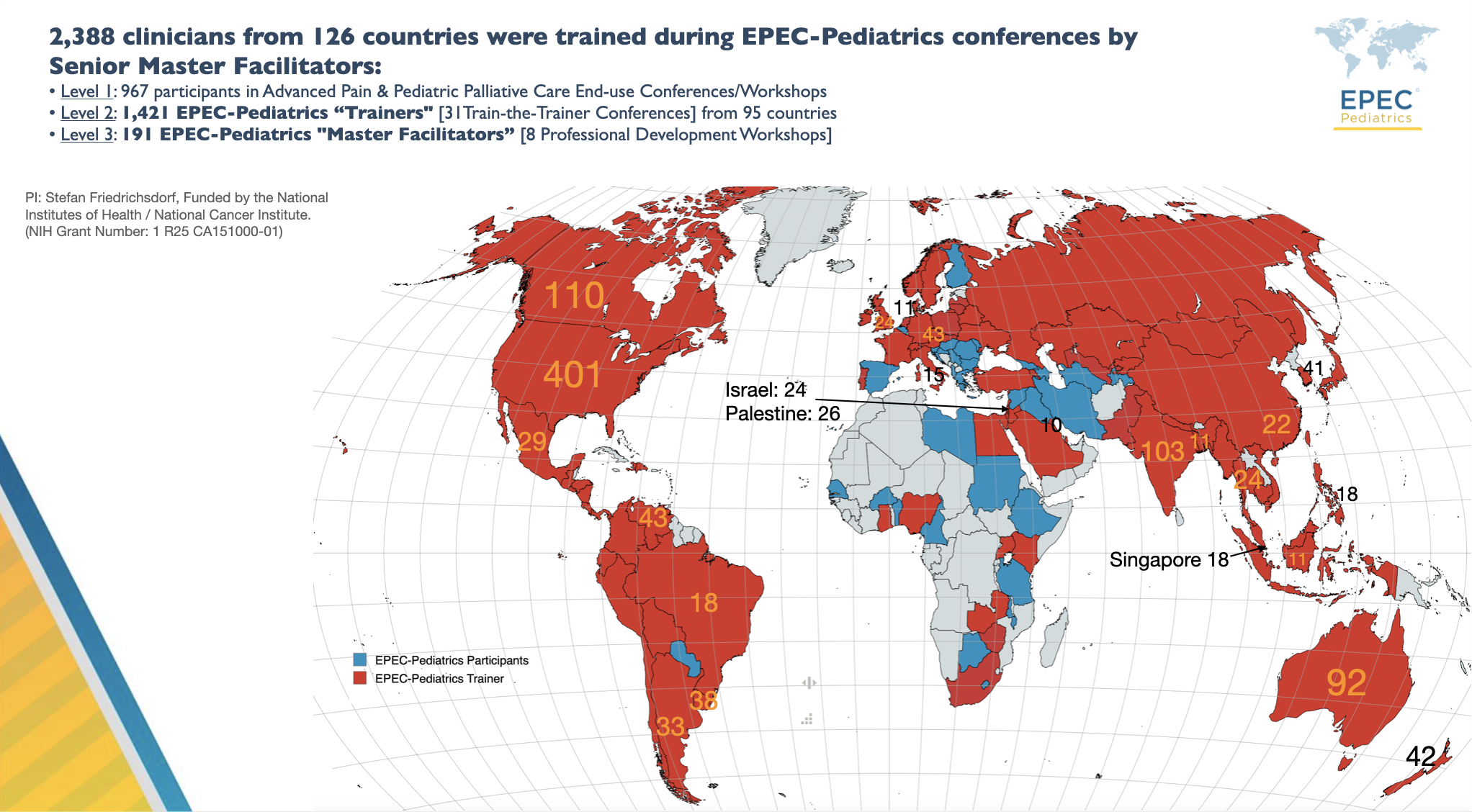 Between 2012-2024 1,421 EPEC-Pediatrics “Trainers" from 95 countries were trained. The map shows countries with 10 or more Trainers.
Between 2012-2024 1,421 EPEC-Pediatrics “Trainers" from 95 countries were trained. The map shows countries with 10 or more Trainers.Figure 2. Location of EPEC Pediatrics Conferences 2012-2024
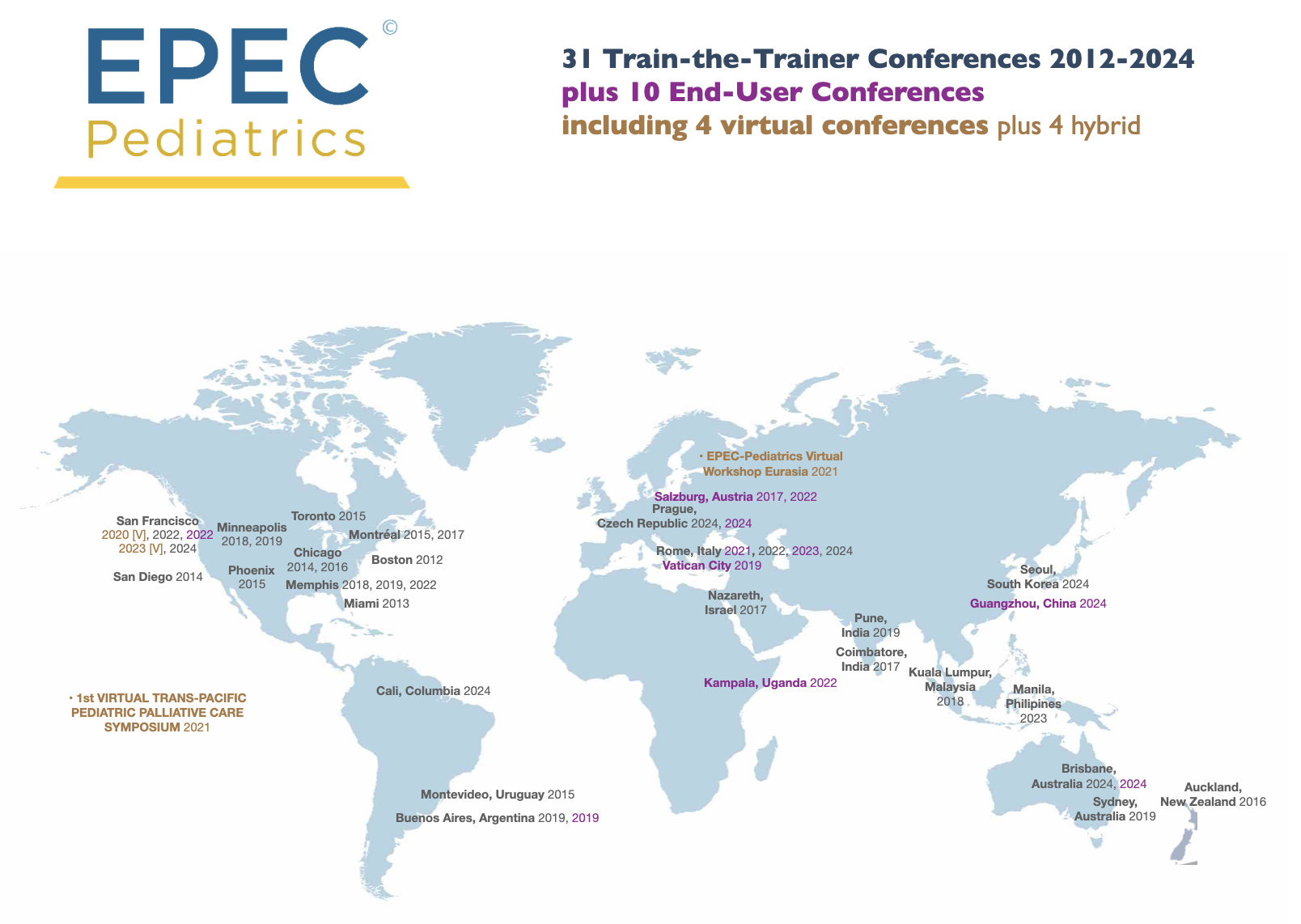
Table 1: Characteristics of EPEC-Pediatrics participants 2019-2023 responding to survey (n=255)
.png)

