Hospital Medicine 6: Clinical
Session: Hospital Medicine 6: Clinical
540 - Characteristics of Infants Hospitalized for Malnutrition and Factors Associated with Readmission
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 540.4262
Emily B. Manion, Phoenix Children's, Phoenix, AZ, United States; Joshua B. Ritzema, Phoenix Children's Hospital, Phoenix, AZ, United States; Minu S. Bhanvadia, Phoenix Children's Hospital, Phoenix, AZ, United States; Sandra Gage, Phoenix Children's Hospital, Racine, WI, United States; Brittany Wold, Phoenix Children’s Hospital, Phoenix, AZ, United States

Emily B. Manion, MD (she/her/hers)
Hospital Medicine Fellow
Phoenix Children's
Phoenix, Arizona, United States
Presenting Author(s)
Background: Children with malnutrition (or failure to thrive) represent ~1.4% to 5% of pediatric hospitalizations, with half estimated to be preventable. One large administrative data study of over 10,000 children under 2 reported a 14% readmission rate, higher in those with complex chronic conditions (CCC) and nasogastric/nasojejunal feeds. However, little is known about these and other factors associated with readmission, specifically in infants under one.
Objective: Describe characteristics of infants under 12 months old admitted for malnutrition and identify factors associated with readmission.
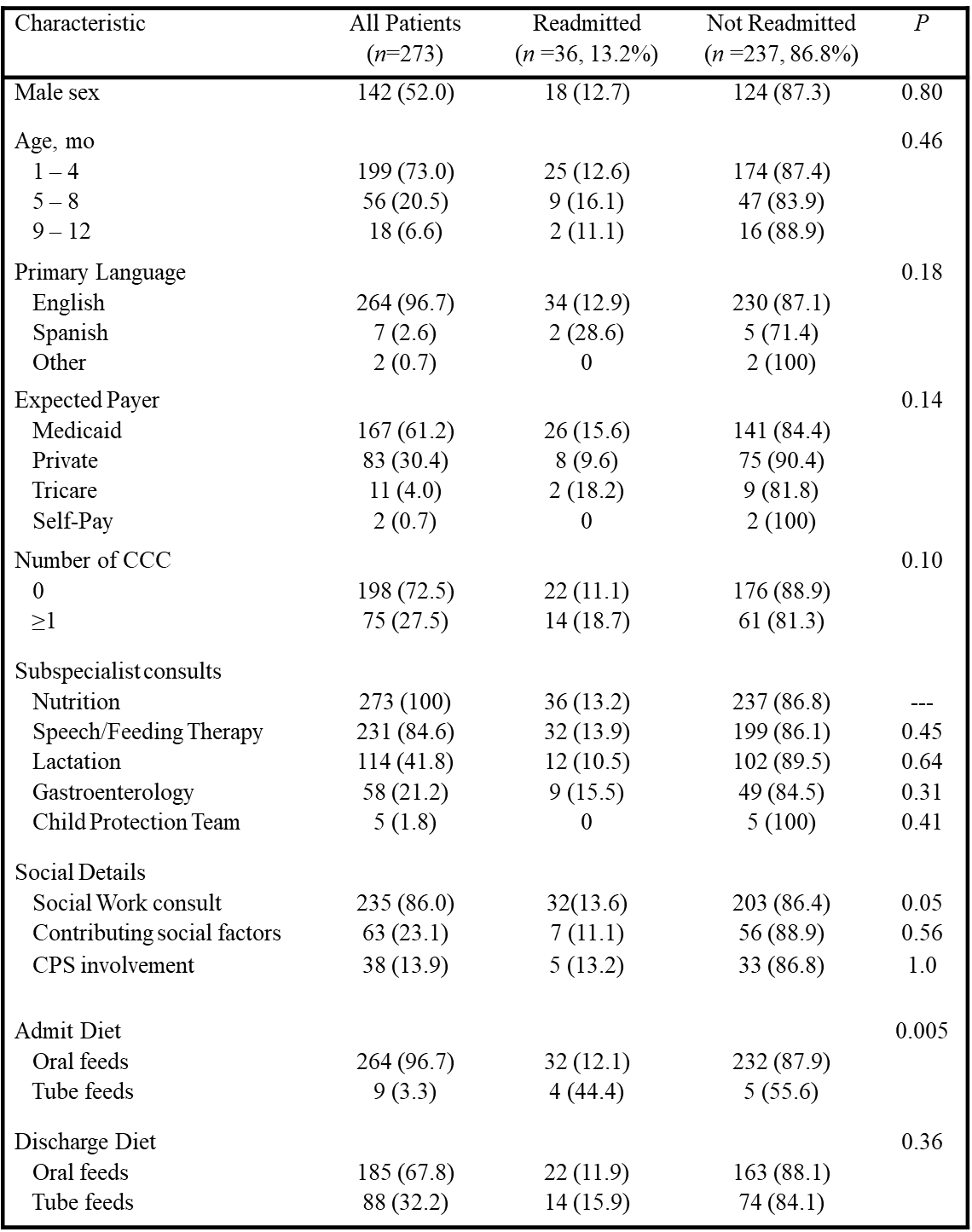
Design/Methods: This IRB-approved retrospective cohort study examined infants 1-12 months old admitted to hospital medicine for malnutrition at a tertiary children’s hospital from 1/2018 to 12/2022. Exclusion criteria: < 36 weeks’ gestation, acute illness. Data collected: demographics, number of CCC, admit/discharge diet, consultations, social factors. Contributing social factors identified in hospitalist and social work notes (Table 1). CCC defined by the 2014 classification system from Feudtner et al. Descriptive statistics used for categorical variables. Associations between characteristics and malnutrition-specific readmissions within 2 years analyzed using χ2 tests, with P values < 0.05 considered statistically significant.
Results: Of 273 infants included, 36 were readmitted (13.5%). Nine infants (3.3%) had tube feeds at admission, and 88 (32.2%) discharged with them. Tube feeds at admission were associated with higher readmission rates (RR) (P=0.005), but tube feeds at discharge were not (Table 2). No demographic factors were associated with readmission. One or more CCC was present in 27.5% of infants, but they had no increased RR. All infants had a nutrition consult; additional consults included speech/feeding therapy (84.6%), lactation (41.8%) and gastroenterology (21.2%); none associated with readmission. Social work was consulted for 86% of infants, identifying social factors in 63 (23.1%), and involving Child Protective Services (CPS) in 38 (13.9%); none associated with increased RR.
Conclusion(s): Our study’s malnutrition-specific readmission rate aligns with existing literature. Factors such as social issues, consultations, and CCC were not associated with increased readmission. Lack of association with CCC may relate to the small number with co-morbidities or undiagnosed conditions in this younger cohort. Infants on tube feeds at admission were more likely to require additional hospitalizations to optimize care. Clinicians should note that these patients may need special consideration in discharge planning.
Table 1: Contributing Social Factors of Infants Admitted for Malnutrition
.png)
Table 2: Demographic and Clinical Characteristics of Infants Admitted for Malnutrition