Endocrinology 1
Session: Endocrinology 1
304 - Hypotonic Versus Isotonic Fluids In Pediatric Diabetic Ketoacidosis
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 304.5308
Rachel Quinn, Vanderbilt University School of Medicine, Nashville, TN, United States; Donald H. Arnold, Vanderbilt University School of Medicine, Nashville, TN, United States; Justin Gregory, Vanderbilt University School of Medicine, Nas, TN, United States

Rachel Quinn, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Vanderbilt University School of Medicine
Nashville, Tennessee, United States
Presenting Author(s)
Background: Physicians most commonly treat children with diabetic ketoacidosis (DKA) using two-bag protocols employing isotonic saline. However, isotonic saline can contribute to hyperchloremic acidosis, potentially prolonging the time to acidosis correction and extending the duration of insulin infusions. To address this, we revised our clinical practice guideline (CPG) in January of 2020, switching from an isotonic to a hypotonic two-bag protocol.
Objective: This study aimed to compare children with DKA managed with the isotonic protocol before January 2020 and those managed with the hypotonic protocol after January 2020. The primary outcome was duration of insulin infusion (in hours), serving as a surrogate marker for the time to acidosis correction. The secondary outcome was hospital length of stay (LOS).
Design/Methods: This is a retrospective study using data from the Epic electronic medical record system. Patients aged 0 to 18 years diagnosed with DKA from November 2017 through September 2024 were included. We excluded patients whose management deviated from the institution’s CPG. For patients with multiple encounters, only the first was analyzed. Data were collected using Epic Clarity database and analyzed using GraphPad (10.4.0) and STATA (14.2).
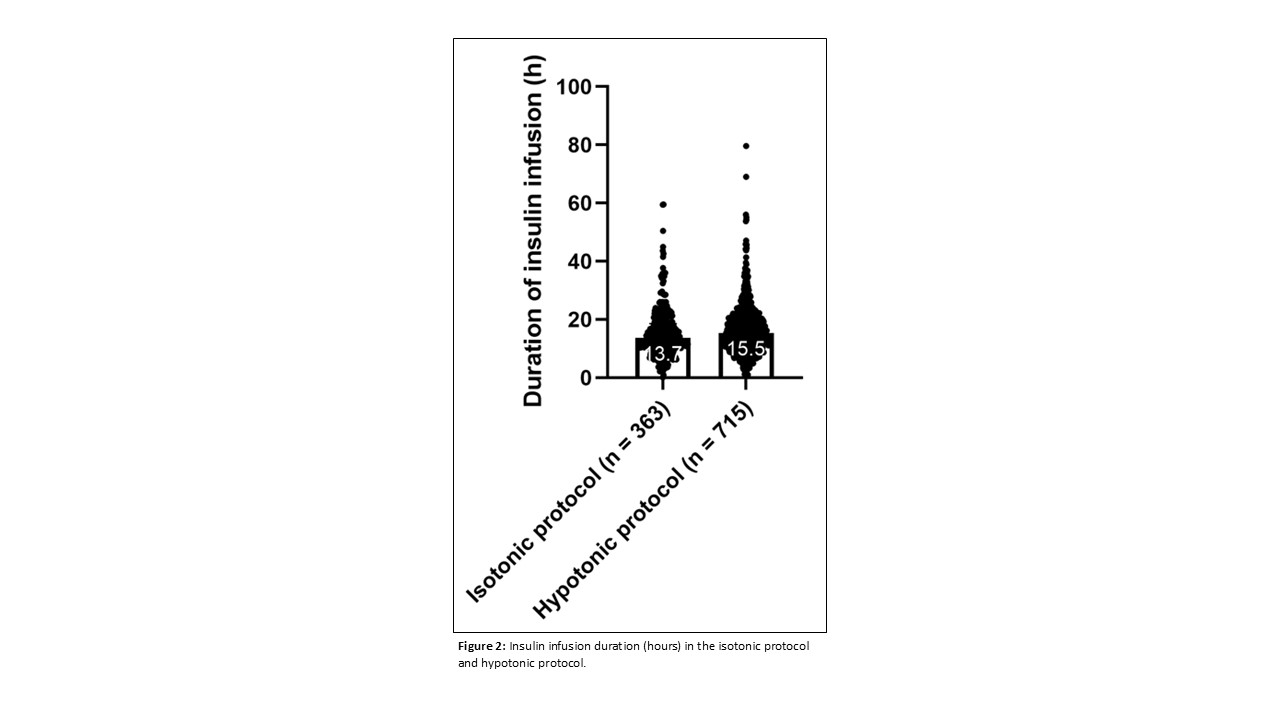
Results: Patient encounters were categorized into the isotonic protocol group (n=363) prior to January 22, 2020, and the hypotonic protocol (n=715) that started on January 22, 2020 (Table 1). In the isotonic group, most patients received fluids with a sodium concentration of 154 mEq/L whereas in the hypotonic group, most received fluids with a sodium concentration of 77 mEq/L (Figure 1). Median insulin infusion duration was 13.73 hours (IQR 10.18-18.65) for the isotonic protocol versus 15.48 hours (IQR 11.2-20.6) for the hypotonic protocol (p=0.0008). Median admission time was 26.38 hours (IQR 20.45-41.78) for the isotonic protocol versus 30.57 hours (IQR 22.43-45.73) for the hypotonic protocol (p= 0.0026). We found no association between infusate sodium concentration and insulin duration in our multivariable linear regression analysis (p=0.62).
Conclusion(s): Our findings are pertinent to endocrinologists, emergency medicine physicians, and intensivists who treat DKA. Contrary to expectations, insulin infusion duration and hospital LOS were longer with the hypotonic protocol. However, our multivariable linear regression analysis found no apparent association between infusate sodium concentration and insulin duration or hospital LOS. Our future research will determine additional factors affecting these outcomes to optimize treatment protocols.
Baseline Patient Characteristics and Data
.jpg)
Sodium Concentrations
.jpg)
Insulin Infusion Duration