Nephrology 5
Session: Nephrology 5
620 - Evaluation of Anticoagulant Methods in Newborns Undergoing Continuous Renal Replacement Therapy: What is the Optimum Method?
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 620.5034
Doğan Kaymaz, Ankara University Faculty of Medicine, Ankara, Ankara, Turkey; Selin Aslan Bayhan, Ankara university children’s hospital, Ankara, Ankara, Turkey; Ezgi Kostekci, Hakkari State Hospital, Ankara, Ankara, Turkey; Ferhan Demirtaş, Ankara University Faculty of Medicine, Ankara, Ankara, Turkey; Ayşen Durak Aslan, Ankara University School of Medicine, Ankara, Ankara, Turkey; Merve Havan, Ankara University, Ankara, Ankara, Turkey; Emel Okulu, Ankara University Faculty of Medicine, Ankara, Ankara, Turkey; Ömer Erdeve, Ankara University School of Medicine, Ankara, Ankara, Turkey; Fatma Begüm Atasay, ankara University, ankara, Ankara, Turkey; Tanıl Kendirli, Ankara University School of Medicine, Ankara, Ankara, Turkey; Saadet Arsan, Ankara University, Ankara, Ankara, Turkey

Emel Okulu, MD (she/her/hers)
Attending Neonatologist, Assoc Prof
Ankara University Faculty of Medicine
Ankara, Ankara, Turkey
Presenting Author(s)
Background: Implementing continuous renal replacement therapy (CRRT) in neonates is technically challenging due to complexities with vascular access, the risk of hemodynamic instability, and the need for precise anticoagulation management. Regional citrate anticoagulation has been shown to manage bleeding risks more effectively than heparin; however, its use in neonates is controversial due to potential adverse effects.
Objective: This study aimed to evaluate the association between anticoagulation methods and the incidence of complications in neonates undergoing CRRT at our facility.
Design/Methods: We conducted a retrospective analysis of the demographic, clinical, and laboratory data of neonates who underwent CRRT from July 2014 to July 2024. Pre-dialysis demographic, clinical, and laboratory characteristics, along with organ failure, coagulopathy risk, and dialysis indications were evaluated in infants receiving regional citrate or heparin anticoagulation. Dialysis daration, filter lifespan, and dialysis-related complications were compared between the two anticoagulation regimens.
Results: A total of 26 patients who received CRRT were included in the study. There were no significant differences between the two groups regarding gestational age, birth weight, dialysis initiation day, dialysis indications, pre-dialysis organ failure, catheter location and size, or dialysis methods employed (p>0.05). The pre-dialysis phosphorus and albumin levels were higher in the regional citrate group (p=0.017, and p=0.02, respectively). Although there was no difference in post-dialysis ionized calcium levels; total calcium, blood urea nitrogen and sodium levels were lower in the regional citrate group (p < 0.05). Dialysis-related bleeding, blood product requirements, thermoregulatory disturbances, infections, inotrope requirements, electrolyte imbalances, and metabolic disturbances during dialysis were comparable between the two groups (p>0.05). A total of 36 dialysis sessions were conducted over 653 hours, with a longer filter lifespan in the regional citrate group compared to the heparin group [18 h (10-19 h) vs. 8 h (3-24 h), p=0.02]. The mean duration of hospitalization was longer in the regional citrate group (p=0.04), while mortality rates were comparable (p=0.13) (Table).
Conclusion(s): The use of regional citrate as an anticoagulant in neonatal CRRT is a safe and effective alternative to heparin. It prolongs filter lifespan without increasing dialysis-related complications. However, further research is necessary to explore the application of regional citrate in the neonatal population.
Table
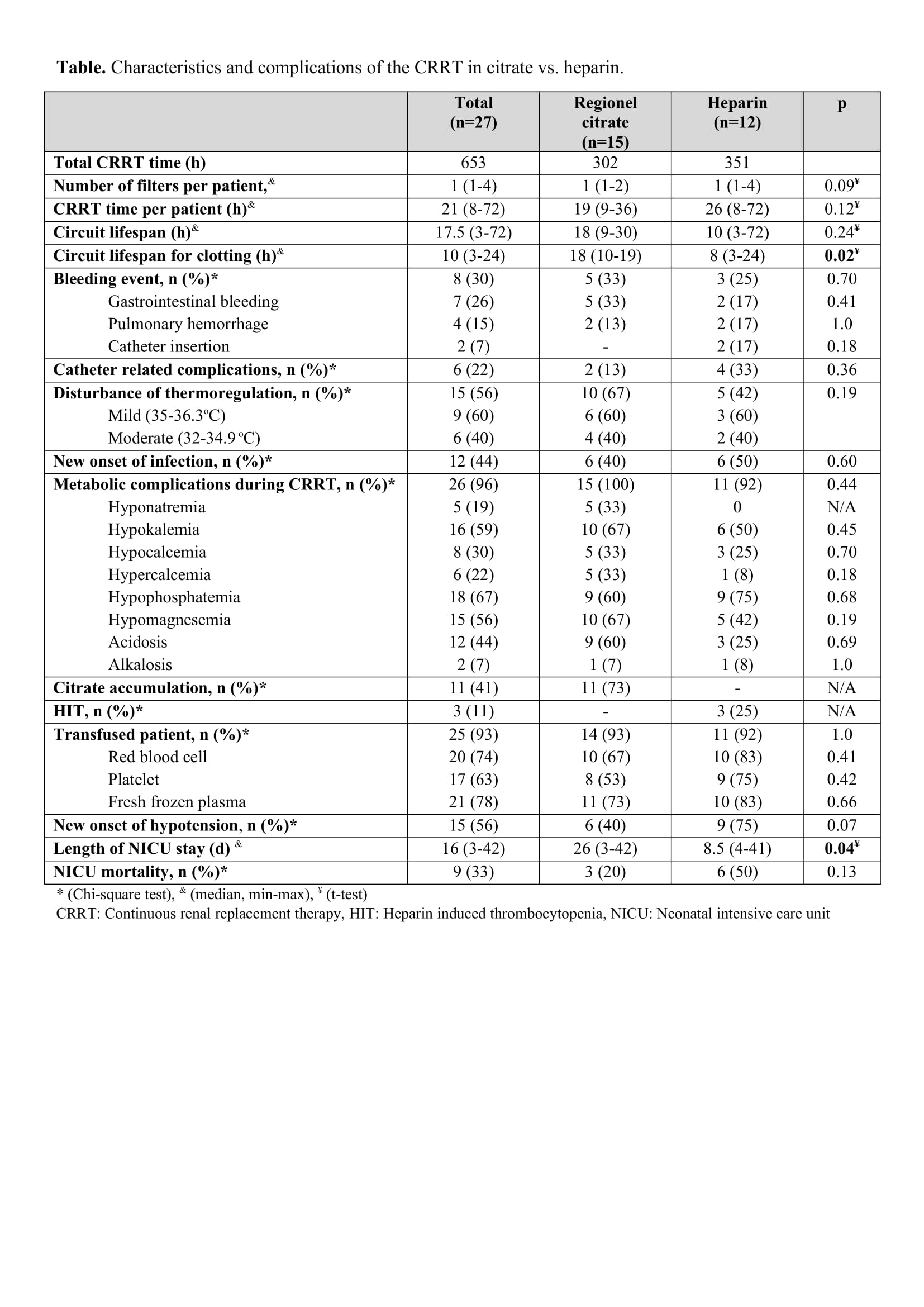 Characteristics and complications of the CRRT in citrate vs. heparin.
Characteristics and complications of the CRRT in citrate vs. heparin.
