Nephrology 2
Session: Nephrology 2
017 - Long-term kidney function and mortality in childhood nephrotic syndrome: a systematic review and meta-analysis.
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 17.5625
Bess-Joan O. Ogome, The Hospital for Sick Children, Toronto, ON, Canada; Cal Robinson, The Hospital for Sick Children, Toronto, ON, Canada; Nithiakishna Selvathesan, The Hospital for Sick Children, Toronto, ON, Canada; Rulan Parekh, Women's College Hospital, Toronto, ON, Canada

Bess-Joan O. Ogome, MBBS
Pediatric Resident
The Hospital for Sick Children
Toronto, Ontario, Canada
Presenting Author(s)
Background: Nephrotic syndrome is one of the most common childhood kidney diseases. Although most children experience a relapsing-remitting course with sustained remission by adulthood, repeated relapses, acute kidney injuries, and immunosuppressive medications may lead to chronic kidney disease (CKD). The risk of CKD among children with steroid-sensitive nephrotic syndrome and minimal change disease is poorly understood.
Objective: Our objective was to determine the long-term incidence of kidney failure, CKD, cancer, and mortality in childhood nephrotic syndrome.
Design/Methods: A systematic literature search was performed on five databases (MEDLINE, EMBASE, CENTRAL, Web of Science, and ClinicalTrials.gov) for English publications from 1970-2024. We included studies that enrolled children with primary (idiopathic) nephrotic syndrome (steroid sensitive and resistant) and reported the incidence of kidney failure, CKD, cancer, or mortality. The methodological quality of each study was assessed using the Joanna Biggs Institute Critical Appraisal Checklist for prevalence studies. Meta-analysis was performed to calculate the cumulative incidence of each outcome.
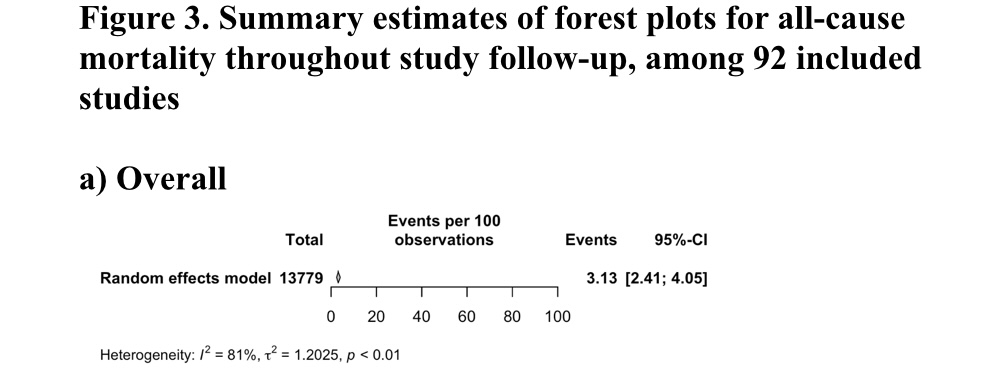
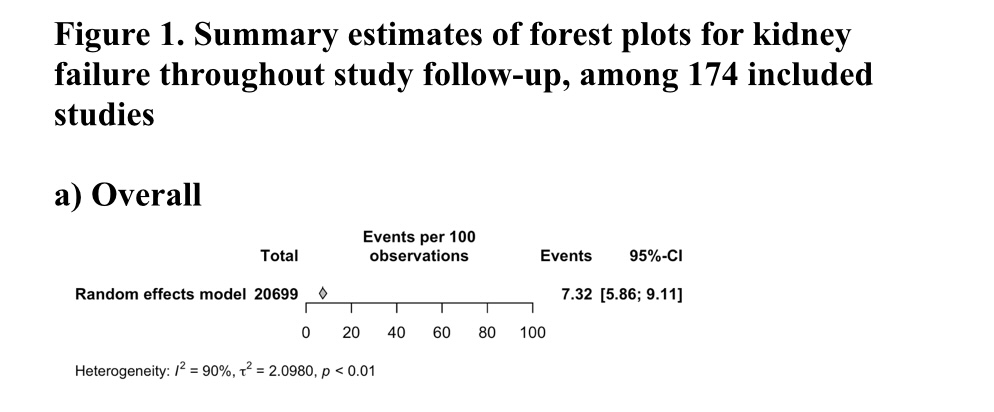
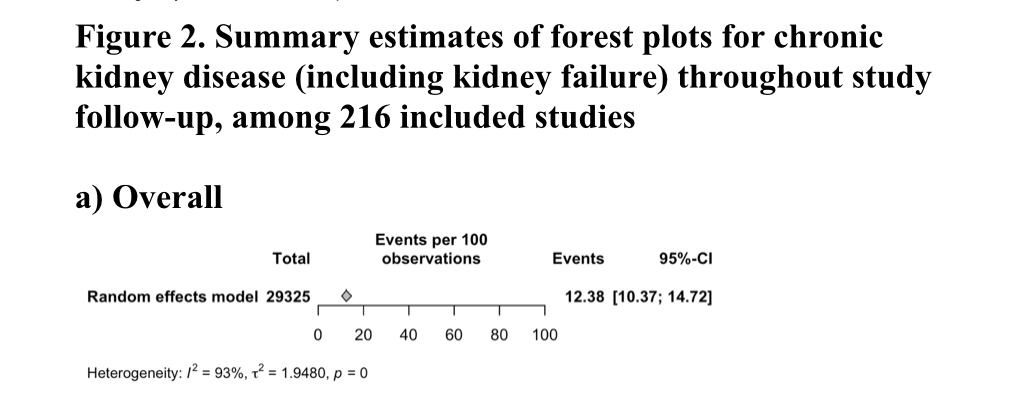
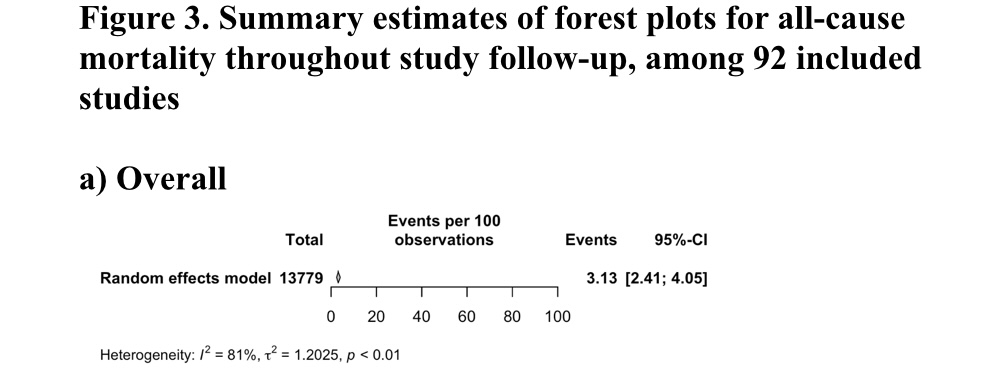
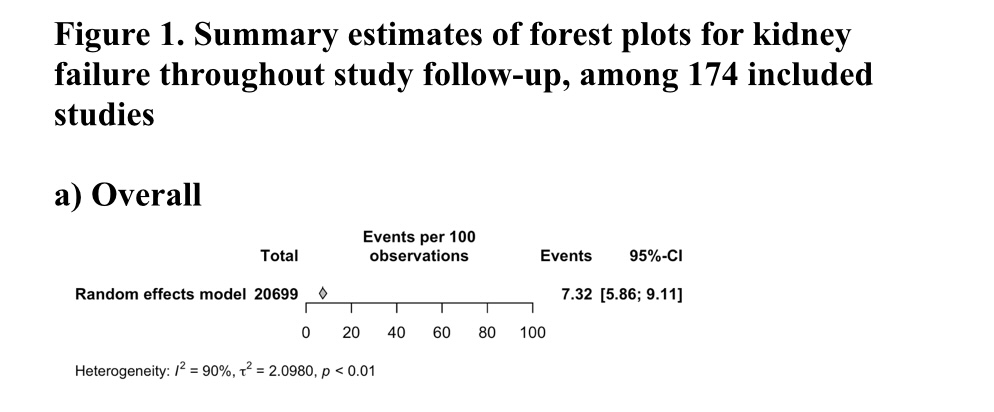
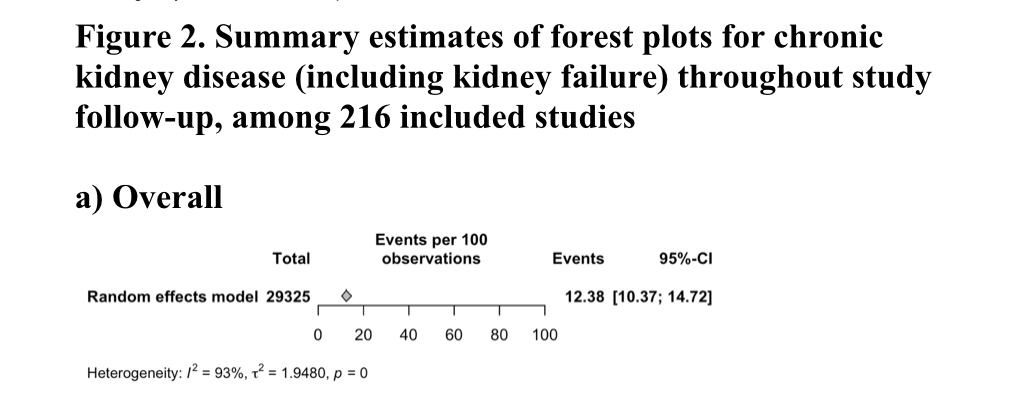
Results: Of 2785 studies screened, 229 were included in this systematic review (32,712 participants). Average follow-up duration was median 5.1 (range 0.3-29) years. The pooled cumulative incidence of kidney failure was 7.3% (95%CI 6.9-9.1). Kidney failure occurred in 13.0% (95%CI 10.3-16.3) of steroid-resistant vs. 0.1% (95%CI 0.0-0.7) of steroid-sensitive children. CKD was assessed in 216 studies (29,325 participants) with a pooled incidence of 12.4% (95%CI 10.4-14.7). Older age at diagnosis, shorter follow-up duration, and North or South American study location were positively correlated with kidney failure and CKD. The pooled incidence of all-cause mortality was 3.1% (95%CI 2.4-4.1). Mortality occurred in 5.0% (95%CI 3.4-7.5) of steroid-resistant vs. 0.9% (95%CI 0.4-2.0) of steroid-sensitive children. The most common causes of death were kidney failure and infections. Cancer occurred in only 16 children in 13 studies (899 participants).
Conclusion(s): Less than 1% of children with steroid sensitive disease developed kidney failure, CKD, or died during study follow-up. Children diagnosed with steroid resistance or focal segmental glomerulosclerosis had significantly higher incidence of kidney failure and death. Close kidney health surveillance and interventions to prevent CKD progression are warranted in these high-risk populations.
Summary estimates of forest plots for kidney failure throughout study follow-up, among 174 included studies.
Summary estimates of forest plots for chronic kidney disease (including kidney failure) throughout study follow-up, among 216 included studies.
Summary estimates of forest plots for all-cause mortality study follow-up, among 92 included studies.
Summary estimates of forest plots for kidney failure throughout study follow-up, among 174 included studies.
Summary estimates of forest plots for chronic kidney disease (including kidney failure) throughout study follow-up, among 216 included studies.
Summary estimates of forest plots for all-cause mortality study follow-up, among 92 included studies.