Nephrology 2
Session: Nephrology 2
019 - Patient and caregiver perspectives on treatment strategies and care priorities of childhood steroid-sensitive nephrotic syndrome: a qualitative study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 19.5798
Augustina Okpere, University of Clagary, Calgary, AB, Canada; Susan M. Samuel, University of British Columbia Faculty of Medicine, Vancouver, BC, Canada; Lorraine Hamiwka, Alberta Children's Hospital, Calgary, Alberta Canada, AB, Canada; Kathryn King-Shier, University of Calgary, Rimbey, AB, Canada; Meghan Elliott, University of Calgary, Calgary, AB, Canada

Augustina Okpere, MBBS, MSc, FWACP (she/her/hers)
Clinical Research Associate
University of Clagary
Calgary, Alberta, Canada
Presenting Author(s)
Background: Approximately 50% of children with steroid-sensitive nephrotic syndrome (SSNS) experience a relapsing and remitting course. Second-line immunosuppressive therapies such as calcineurin inhibitors, mycophenolate, cyclophosphamide, and rituximab, are considered if steroids alone cannot sustain remission or to minimize cumulative steroid-related toxicity. However, these therapies expose patients to additional potential risks such as infertility, malignancy, chronic kidney disease, and gingival overgrowth without compelling evidence of superiority relative to steroid use or standardized protocols guiding their use across centres. These complexities lead to highly variable SSNS treatment approaches across kidney care providers and programs and pose challenges for maintaining quality of life among affected children.
Objective: We explored the experiences of treatment strategies for SSNS and care priorities among children living with the condition and their caregivers.
Design/Methods: We conducted semi-structured interviews with a purposive sample of children aged 8 to 18 years with SSNS and their caregivers from a pediatric nephrotic syndrome cohort in Southern Alberta, Canada. Using reflexive thematic analysis, we coded transcripts in duplicates and developed themes that integrated key concepts across roles.
Results: Twenty-eight individuals (10 children and 18 caregivers) participated in this study. All had experience of a nephrotic syndrome relapse after initial diagnosis and steroid treatment. Participants identified how their experiences with SSNS treatments influenced their willingness to accept further steroids and other second-line agents. Findings are elaborated across the following 4 themes: (1) Reluctant acceptance of steroids (steroid aversion, lack of personalized steroid dosing, altered self-regulation, acknowledging steroid effectiveness); (2) Coping with unexpected relapses (repeating the cycle, restricted life participation, tempered optimism); (3) Uncertainty about second-line therapies (striving for stability, burden of adverse effects, exploring alternatives); and (4) Directing attention to unmet treatment needs and priorities (mechanistic approaches to therapy, steroid minimization, child and family involvement, enhanced social supports).
Conclusion(s): Children with SSNS and their caregivers expressed a dislike of steroids and desire for individualized treatment protocols. Investigation into therapeutic alternatives for SSNS treatment should integrate patients’ preferences, values, and care priorities
Thematic schema depicting the relationship between main themes. Concerns about steroids and uncertainty about the efficacy and potential consequences of second-line therapies influenced decision making for treatment of disease relapses and, ultimately, contributed to participants’ priorities for management of childhood steroid-sensitive nephrotic syndrome
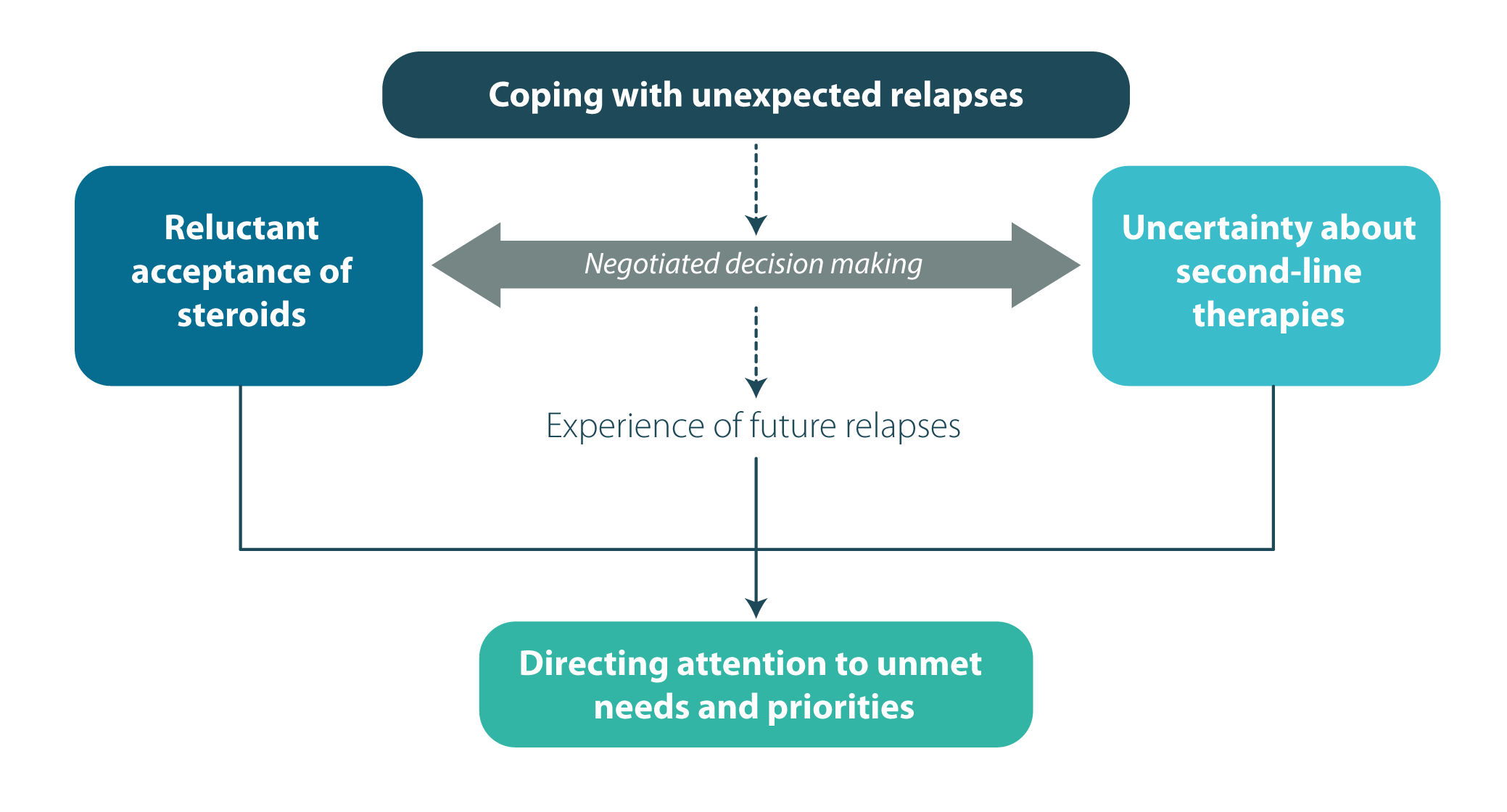 Thematic schema depicting the relationship between main themes. Concerns about steroids and uncertainty about the efficacy and potential consequences of second-line therapies influenced decision making for treatment of disease relapses and, ultimately, contributed to participants’ priorities for management of childhood steroid-sensitive nephrotic syndrome
Thematic schema depicting the relationship between main themes. Concerns about steroids and uncertainty about the efficacy and potential consequences of second-line therapies influenced decision making for treatment of disease relapses and, ultimately, contributed to participants’ priorities for management of childhood steroid-sensitive nephrotic syndrome
