Nephrology 1
Session: Nephrology 1
007 - Psychosocial Barriers to Pediatric Preemptive Kidney Transplantation.
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 7.6192
Judith S. VanSickle, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Darcy K.. Weidemann, Children's Mercy Hospital, Kansas City, MO, United States; Bradley A. Warady, Children's Mercy, Kansas City, MO, United States
- JV
Judith S. VanSickle, MD, MHPE, FAAP, FASN (she/her/hers)
Associate Professor of Pediatric Nephrology
Children's Mercy Hospitals and Clinics
Kansas City, Missouri, United States
Presenting Author(s)
Background: Preemptive Kidney transplantation (PKT) is recognized as the optimal treatment for improving life expectancy and quality of life in children with end-stage kidney disease (ESKD). However, barriers to PKT persist, with insufficient attention given to family social support (FSS) and the impact of psychosocial factors.
Objective: Inadequate FSS and other psychosocial factors negatively impact access to PKT in pediatric ESKD.
Design/Methods: Single-center, retrospective review of 177 pediatric ESKD between 2010 to 2020. Demographic and clinical data as well as detailed, socioeconomic (SES) analysis including Child Opportunity Index (COI), number of caregivers (CG)), and results of 165 psychology evaluations (PE), which were reviewed to identify potential barriers to PKT based on 5 standardized questions: 1- Adequate Knowledge (AK) = adequate knowledge about transplant, 2 -AT = ability to adhere to the treatment based on previous history, Psych= relevant mental health issues impacting transplant success in both parents or child and adequate FSS to help with coping. To increase study power, race was divided into white (W) and non-white (NW). Independent T-test was utilized to compare groups. Univariant then multinominal stepwise logistic regression was conducted to determine whether odds of PKT varied based on findings of the PE after adjustment for known clinical and demographic risk factors.
Results: Relevant clinical and demographic characteristics can be seen in Table 1. 19.3 % of children received PKT. Children with PKT had a shorter time before transplant referral (p= < 0.003), a higher percentage of LD-KT (p < 0.001), and more CGs (p= < 0.001). COI status did not correlate with PKT. From the 5 standardized PE questions, AT, FSS, and Psych in child were the only significant barriers to receiving a PKT (p=0.017, p=0.001, as well 0.03 respectively) (Table 2.). No significant difference in CG between W/NW (p=0.158), but inadequate FSS was more likely among NW (p=0.01), and families who lived in low COI areas (p < 0.001). However, Psych. in the child did not correlate with R (p=0.54) or COI (p=0.67). All SES and PE variables were analyzed in stepwise logistic regression to assess whether they predicted the receipt of PKT. Only FSS (p=0.048) and Psych child (p=0.032), were predictive of receiving PKT.
Conclusion(s): Family support systems and comorbid mental health disorders substantially affect access to PKT. Early intervention and family-centered care can enhance equity in pediatric KT. Understanding and addressing these barriers are critical for optimizing outcomes and enhancing holistic care approaches.
Table 1. Demographic data and characteristic of 177 children with ESKD cared by our center between 2010-2020
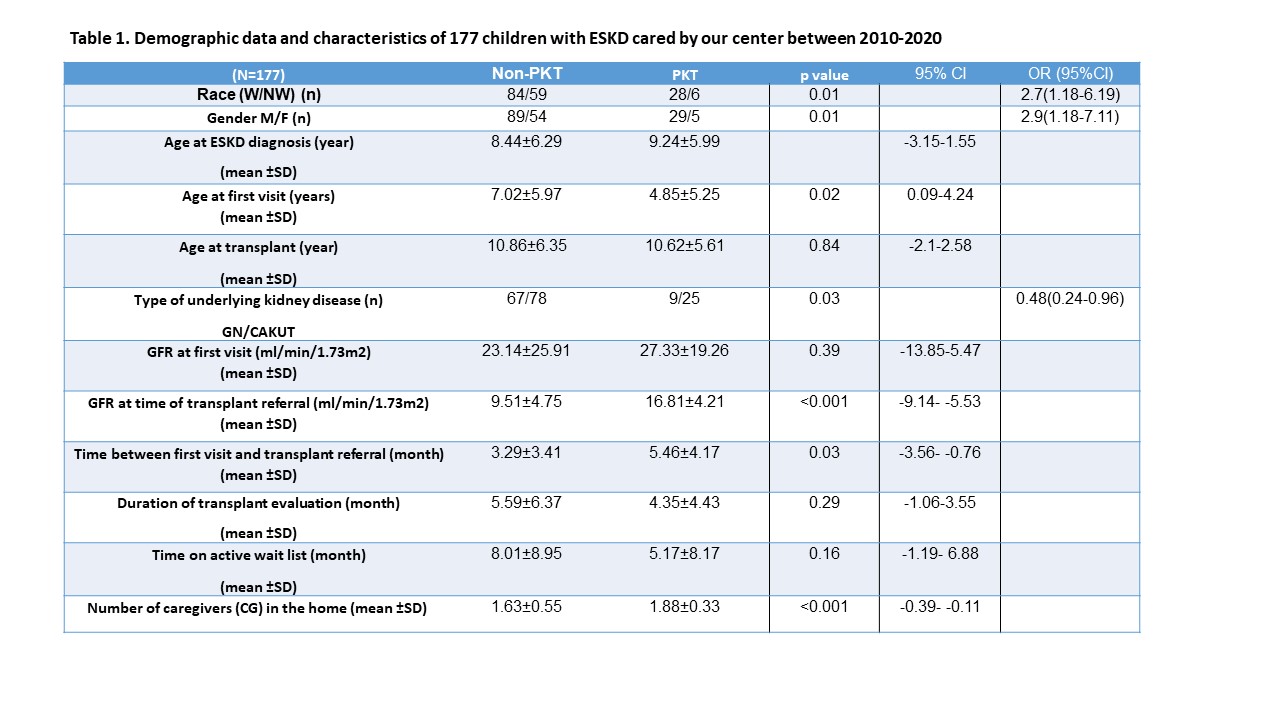 Table 1. Demographic description of ESKD patients per modality. PKT: pre-emptive kidney transplant. Non-PKT: dialysis only + dialysis followed by kidney transplant. Independent test
Table 1. Demographic description of ESKD patients per modality. PKT: pre-emptive kidney transplant. Non-PKT: dialysis only + dialysis followed by kidney transplant. Independent test and Χ-square test.
GFR: glomerular filtration rate, calculated by bedside Schwartz formula.
W: white. NW: non-white. GN: glomerulonephritis. CAKUT: congenital anomaly of the kidney and urogenital system
Table 2. Univariate analysis of the psychosocial factors as predictors of PKT in our cohort
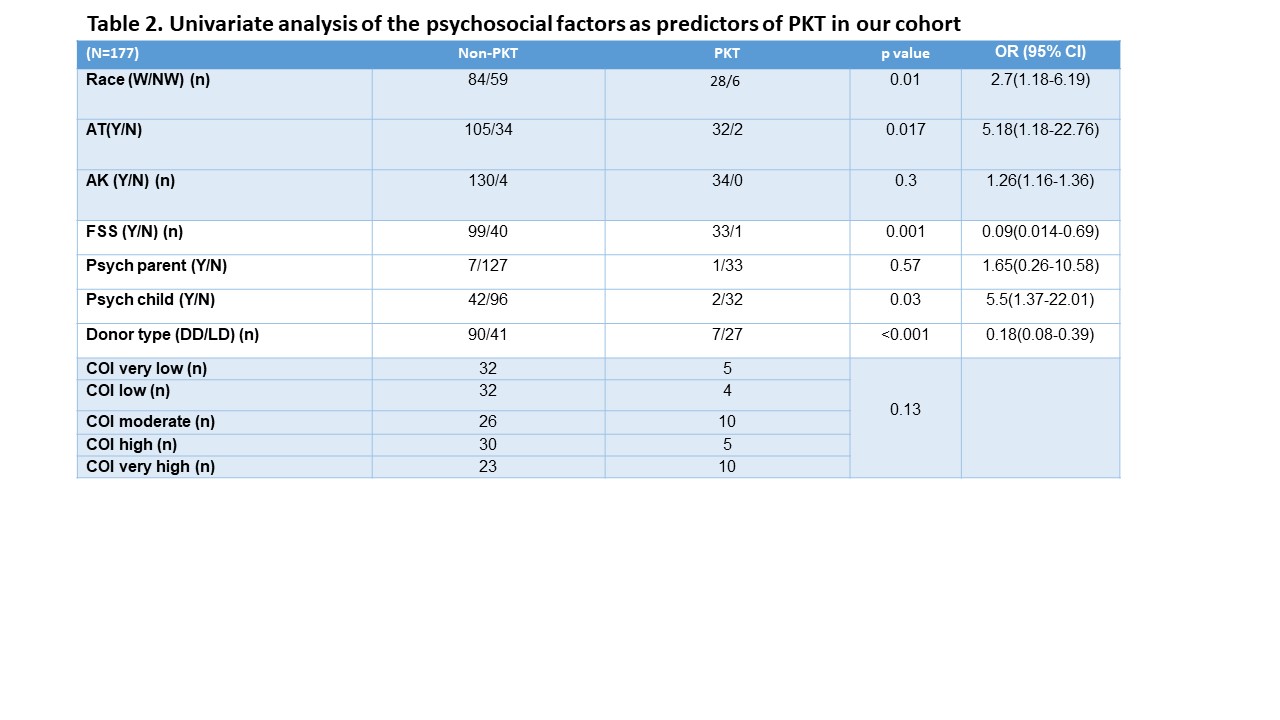 Table 2. Univariate statistical analysis of all variables as predictors of PKT by Chi-square test., p< 0.05.
Table 2. Univariate statistical analysis of all variables as predictors of PKT by Chi-square test., p< 0.05.PKT: Pre-emptive kidney transplant. Non-PKT: dialysis +dialysis followed by kidney transplant. DD: Deceased donor. LD: living donor. AT: Ability to adhere to treatment. AK: Adequate knowledge of the transplant process. FSS: Family social support to help with copying. Psych parent: Psychiatric condition in parent. Psych child: Psychiatric condition in child. COI: Neighborhood Child Opportunity Index
Table 3. Modeling with multinominal logistic regression analysis for predicting Pre-emptive kidney transplant in our cohort
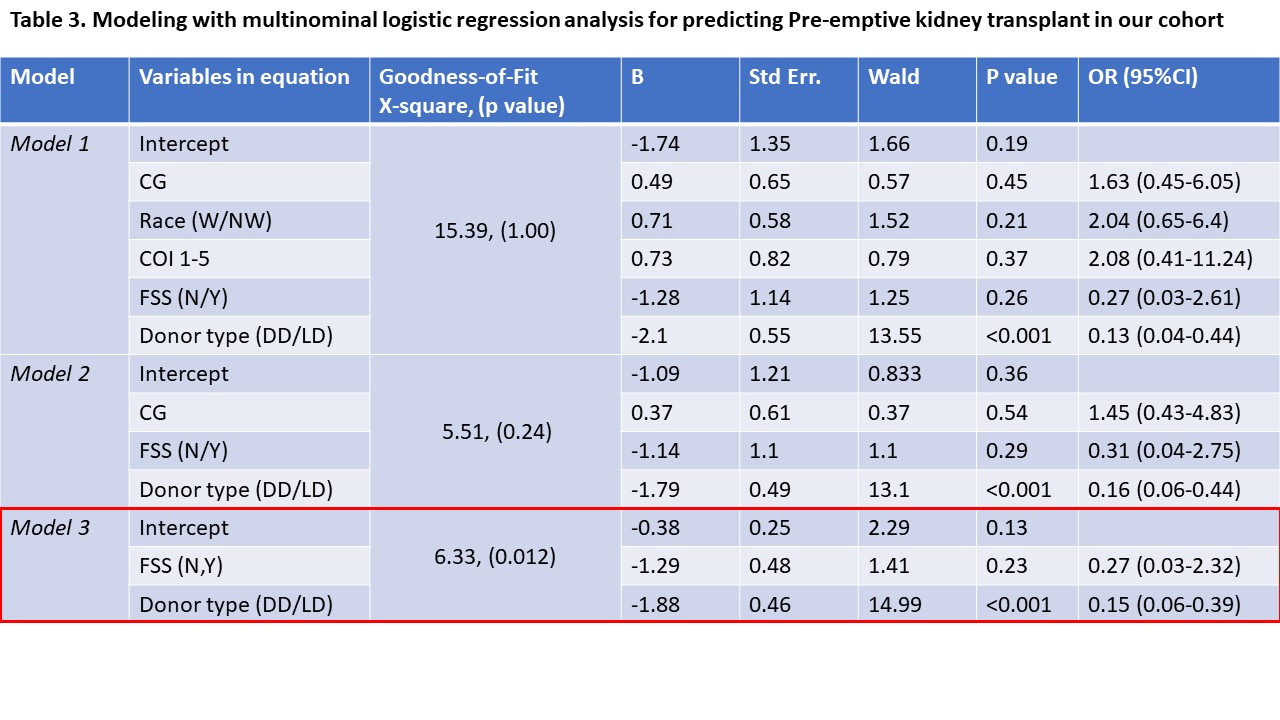 Three models of multinominal logistic regression to evaluate the predictive value of CG, Race, COI 1-5, FSS, and Donor type for PKT.
Three models of multinominal logistic regression to evaluate the predictive value of CG, Race, COI 1-5, FSS, and Donor type for PKT. Model 3 shows the best fit, with LD being a significant predictor of PKT. Multinominal regression analysis, p< 0.005).
PKT: pre-emptive kidney transplant. Non-PKT: Dialysis + Dialysis followed by kidney transplant. CG: number of caregiver in the home. W: white, NW: non-white. FSS: family social support. DD: deceased donor. LD: living related donor

