Nephrology 6
Session: Nephrology 6
635 - Provider Perspectives on the Role of Hypotension in Pediatric Kidney Transplant: A Pediatric Nephrology Research Consortium Study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 635.6167
Hailey Connolly, Joseph M. Sanzari Children's Hospital Hackensack University Medical Center, Jersey City, NJ, United States; Olga Charnaya, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Sruthi Tatavarthi, Johns Hopkins University, Ellicott City, MD, United States; Shireen Hashmat, University of chicago, Chicago, IL, United States
- HC
Hailey Connolly, MD (she/her/hers)
Resident Physician
Joseph M. Sanzari Children's Hospital Hackensack University Medical Center
Jersey City, New Jersey, United States
Presenting Author(s)
Background: Persistent pre-transplant hypotension is commonly recognized as a unique and significant cause of morbidity in pediatric kidney transplantation, however there is minimal data in the literature on impact or management of this complication. Studies have been hampered by lack of a consistent definition, low sample size at individual institutions, and high variability in clinical practice.
Objective: The aim of this study is to describe the clinical definition of pre-transplant hypotension, identify the common etiologies seen in clinical practice, and detail the different treatment modalities used for the management of pre- and post-transplant hypotension derived from surveys of practicing kidney transplant clinicians.
Design/Methods: A 10-question survey was approved by the Clinical Research Review Committee of the Pediatric Nephrology Research Consortium (PNRC) and distributed to pediatric nephrologists. The survey data was analyzed using descriptive statistical methods in STATA version 17 without hypothesis testing. This study received exempt status from the University of Chicago IRB.
Results: Twenty-five pediatric nephrologists responded to the survey. The most common definitions for hypotension were systolic blood pressure less than the 5th (32%) or 10th percentile (28%) (Figure 1). Common etiologies for hypotension included vasoplegia, anephric status, dialysis-associated hypotension, and cardiac pathology. Most nephrologists (92%) preferred peritoneal dialysis for patients with pre-transplant hypotension. The majority (76%) referred hypotensive patients for transplant listing and had treated hypotension with pharmacologic interventions including midodrine, fludrocortisone, and sodium chloride (Figure 2). In the first 24-48 hours post-transplant, blood pressure goals varied, with the most common lower limit for systolic blood pressure set above the 50th percentile. The pharmacologic agents used for management of post-transplant hypotension also differed among respondents (Figure 2).
Conclusion(s): There is significant variability in practice patterns regarding the management of hypotension in pediatric kidney transplant recipients. Survey results highlight the lack of a consistent definition for hypotension and differences in management during pre- and post-transplant periods, reinforcing the need for standardized clinical care guidelines. Further studies are needed to evaluate the scope of chronic hypotension in the pediatric nephrology population and determine its impact on patient and allograft survival.
CV 2024.pdf
Figure 2: Distribution of therapies utilized for hypotension
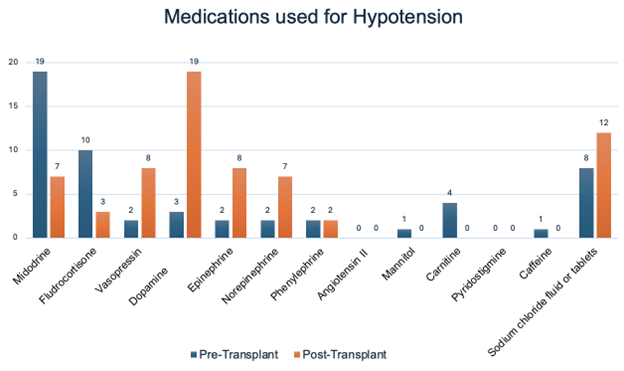 Respondents were asked to select all medications that they used in their practice. In the pre-transplant phase, Midodrine and Fludrocortisone were the most commonly used therapies, with 19 and 10 respondents respectively, while dopamine and vasopressin were less frequently utilized. Post-transplant, dopamine and epinephrine emerged as the most used therapies with 19 and 8 respondents respectively, indicating a shift in medication preferences following the transplant.
Respondents were asked to select all medications that they used in their practice. In the pre-transplant phase, Midodrine and Fludrocortisone were the most commonly used therapies, with 19 and 10 respondents respectively, while dopamine and vasopressin were less frequently utilized. Post-transplant, dopamine and epinephrine emerged as the most used therapies with 19 and 8 respondents respectively, indicating a shift in medication preferences following the transplant.CV 2024.pdf
Figure 2: Distribution of therapies utilized for hypotension
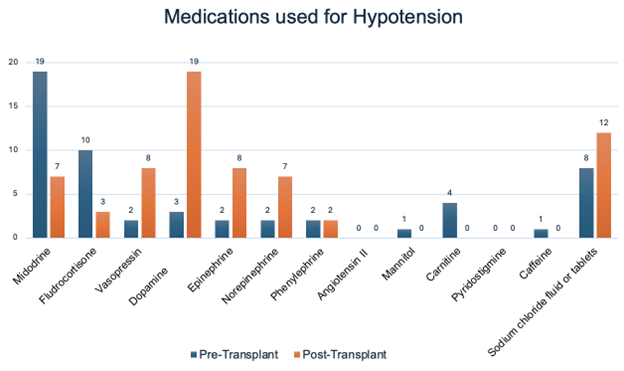 Respondents were asked to select all medications that they used in their practice. In the pre-transplant phase, Midodrine and Fludrocortisone were the most commonly used therapies, with 19 and 10 respondents respectively, while dopamine and vasopressin were less frequently utilized. Post-transplant, dopamine and epinephrine emerged as the most used therapies with 19 and 8 respondents respectively, indicating a shift in medication preferences following the transplant.
Respondents were asked to select all medications that they used in their practice. In the pre-transplant phase, Midodrine and Fludrocortisone were the most commonly used therapies, with 19 and 10 respondents respectively, while dopamine and vasopressin were less frequently utilized. Post-transplant, dopamine and epinephrine emerged as the most used therapies with 19 and 8 respondents respectively, indicating a shift in medication preferences following the transplant.
