Nephrology 6
Session: Nephrology 6
632 - The Prevalence and Impact of Food Insecurity in Pediatric Patients with Chronic Kidney Disease (CKD), Including Those On Dialysis and Post-Transplant
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 632.6881
Rafaella Faria, Johns Hopkins Children's Center, Baltimore, MD, United States; Yu Bin Na, Johns Hopkins University School of Medicine, Baltimore City, MD, United States; Laura Prichett, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Cozumel Pruette, Johns Hopkins University School of Medicine, Baltimore, MD, United States

Rafaella Faria, MD (she/her/hers)
Resident Physician
Johns Hopkins Children's Center
Baltimore, Maryland, United States
Presenting Author(s)
Background: Food insecurity affects 12.5% of households with children in the US, and is associated with increased healthcare utilization, worse weight outcomes, increased rates of high blood pressure, and other poor health outcomes in children. Limited research exists on the prevalence and impact of food insecurity in the CKD population. Prior studies suggest the prevalence of food insecurity in children with kidney disease is higher than in the general population, and restrictive diet recommendations can contribute to food insecurity. There are currently no studies that have included the full spectrum of patients with CKD, including patients on dialysis and post-transplant.
Objective: To determine the prevalence of food insecurity in pediatric patients (age 1d-22 yrs) with CKD, including those on dialysis and post-transplant. We explored associations between food insecurity and demographic data, hypertension, potassium and phosphorus levels, prescription of potassium and phosphorus binders, medication burden, and growth metrics.
Design/Methods: An observational, retrospective single site study. Food insecurity was assessed with the Hunger Vital Sign in patients with CKD seen at a tertiary academic center. This study was IRB exempt.
Results: The prevalence of food insecurity varied, with 9% of patients with CKD not on dialysis, 19% of patients on dialysis, and 6% of patients post-transplant being food insecure. Food insecure patients were more likely to be of black or African American race (p = 0.003) and to be hyperphosphatemic (p= 0.01). There were no statistically significant associations between food insecurity and other outcomes of interest.
Conclusion(s): The prevalence of food insecurity in kids with CKD varies, with patients on dialysis having a higher prevalence than those not on dialysis and post-transplant. Children on dialysis may be at higher risk for food insecurity given financial and time constraints placed on caregivers and more restrictive diet recommendations. Children with food insecurity in our population were more likely to be of black or African American race, though we were not able to account for confounders in this study. Food insecurity was associated with hyperphosphatemia, potentially due to phosphorus being present in many preservatives in shelf-stable, cheaper food options. This study highlights the importance of routine screening for food insecurity in children with CKD, as both dialysis and transplant may affect food security status, dietary restrictions may not be feasible for food insecure families, and those with food insecurity may require closer phosphorus level monitoring.
Certification of Trainee Status
Rafi Certification Letter PAS Genies.pdf
Figure 1: Prevalence of Food Insecurity Stratified by CKD Status
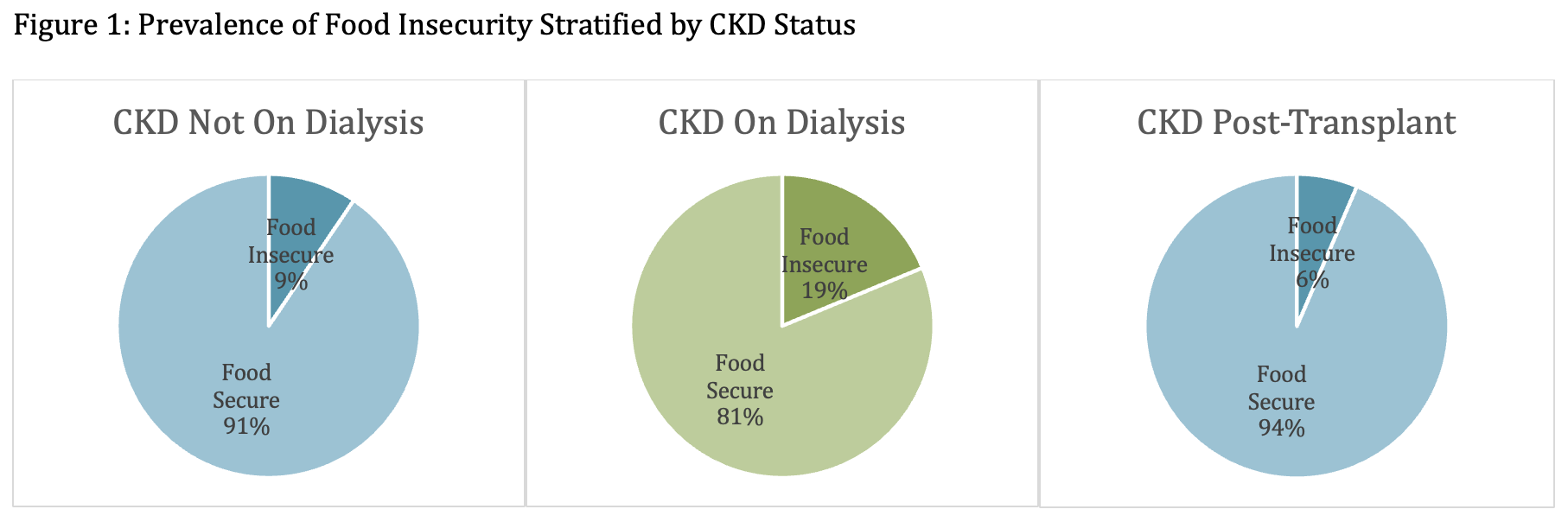
Table 2. Health Metrics Stratified by Food Security Status
.png)

