Nephrology 1
Session: Nephrology 1
010 - HLA-DQ De Novo Donor Specific Antibodies are Associated with Graft Failure in Pediatric Kidney Transplant Recipients
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 10.5302
Anika Shah, University of Wisconsin Madison, Madison, WI, United States; Vaka Sigurjonsdottir, University of Miami, Stanford, CA, United States; Daniel Turudic, University Hospital Centre Zagreb, Zagreb, Grad Zagreb, Croatia; Paul Grimm, Stanford University, Medical S, Palo Alto, CA, United States; Bing M. Zhang, Stanford University School of Medicine, Palo Alto, CA, United States
.jpg)
Anika Shah (she/her/hers)
Student
University of Wisconsin Madison
Sunnyvale, California, United States
Presenting Author(s)
Background: De novo anti-HLA-DQ donor specific antibodies (dnDSA) have been shown to be the most common antibodies associated with lower graft survival compared to all other HLA loci
Objective: This study aimed to investigate the impact of HLA-DQ and HLA-DR dnDSA on graft outcomes in pediatric kidney transplant recipients.
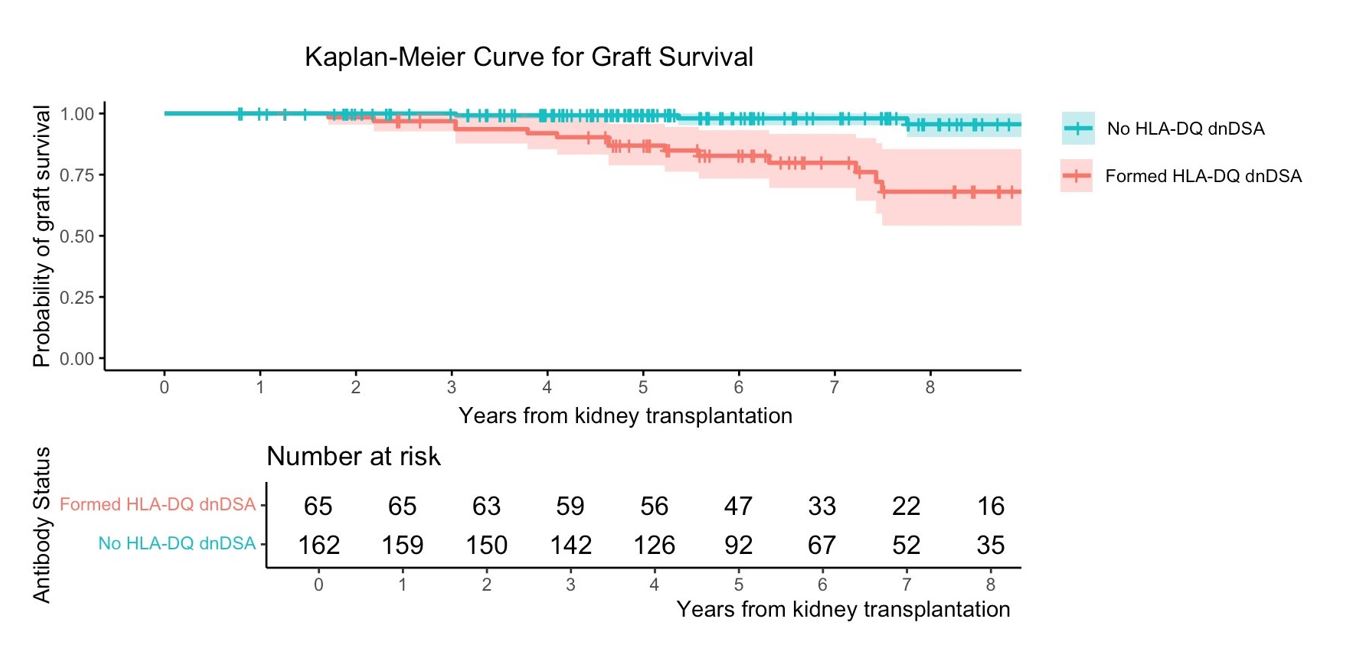
Design/Methods: Children who underwent kidney transplantation from 1/1/2010-3/1/2018 at Stanford, with at least 12-month follow-up, were included and followed through 9/1/2022. High-resolution HLA typing was performed using next generation sequencing. DQα/β heterodimers were paired based on linkage disequilibrium with HLA-DRB1 and mismatches were determined at the level of the heterodimers. A risk mismatch was defined as the presence of DQα05 heterodimer in donor, not in recipient. Primary outcome was the development dnDSA to HLA-DQ and HLA-DR, defined as ≥ 3000 mean fluorescence intensity (MFI) by the IgG assay. All patients were tested for dnDSA at time 0, 1-, 2-, 3-, 6-, and 12-months post-transplant, at least annually thereafter, and as clinically indicated. Biopsies were scored by an expert in pathology per the most recent Banff criteria. Fisher’s exact test was used to compare groups. Survival analysis was performed with the Kaplan-Meier method using the log-rank test for significance. Cox Proportional Hazards Survival Regression was performed.
Results: A total of 227 patients were included. Of those, median age was 14 (IQR 4-17), 24% had living donor transplant, 49% were female and majority was of Hispanic/Latino origin (39%). The median follow-up time was 73 (IQR 58-96) months. A total of 65 (29%) patients formed anti-HLA-DQ dnDSA and 36 (16%) formed anti-HLA-DR dnDSA. Of those who formed dnDSA to DR, 28 (78%) also formed dnDSA to DQ. Complement-binding dnDSA was more common for DQ than DR, 46 (71%) vs 10 (27%), p< 0.001. C1q positive anti-DQ dnDSA was associated with adverse graft outcomes, HR 2.7 (95% CI, 1.66-4.55) , p< 0.001. C1q positive anti-DR dnDSA was not significantly associated with adverse graft outcomes, p=0.35. Graft outcomes were worse in patients forming anti-DQ dnDSA, Figure, table. Risk heterodimer mismatch was associated with HLA-DQ dnDSA formation, table. Predicted Indirectly Recognizable HLA Epitopes (PRICHE-II) scores were a better predictor of immunological risk than single eplet mismatch load, table.
Conclusion(s): HLA-DQ dnDSA was more common and associated with worse graft outcomes than HLA-DR dnDSA. Better matched kidneys specifically at the HLA-DQ allele level with an understanding of immunogenic mismatches may improve graft outcomes and decrease sensitization.
Table
.jpg)
Figure