Emergency Medicine 8
Session: Emergency Medicine 8
118 - Oxygen saturation characteristics in young infants with bronchiolitis
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 118.5616
Son H. McLaren, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Murad Megjhani, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Carlos A. Camargo, Mass General Hospital / Harvard University, Boston, MA, United States; Joseph R. Isler, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Marlin Morel, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Tania Pakholok, Columbia University Vagelos College of Physicians and Surgeons, Brooklyn, NY, United States; Cheng-Shiun Leu, Columbia University, New York, NY, United States; Jiying Han, Columbia University, New York, NY, United States; Daniel Fenster, Columbia University Vagelos College of Physicians and Surgeons, Scarsdale, NY, United States; Daniel Green, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Katie A. Friedman, NewYork-Presbyterian Morgan Stanley Children's Hospital, NEW YORK, NY, United States; Tammam Alalqum, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Vanessa M. Lorenzo, NewYork-Presbyterian Morgan Stanley Children's Hospital, bridgeport, CT, United States; Todd A. Florin, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Asuncion Mejias, St. Jude Children's Research Hospital, Memphis, TN, United States; Soon Bin Kwon, Columbia University Vagelos College of Physicians and Surgeons, Fort Lee, NJ, United States; Bennett Weinerman, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Benjamin L. Ranard, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Daniel Nametz, Columbia University Irving Medical Center, New York, NY, United States; Peter Dayan, Columbia University, Hastings on Hudson, NY, United States; Soojin Park, Columbia University Medical Center/NY Presbyterian Hospital, New York, NY, United States
- PD
Peter Dayan, MD, MSc (he/him/his)
Director of Research, Pediatric Emergency Medicine
Columbia University
Hastings on Hudson, New York, United States
Presenting Author(s)
Background: Various pulse oximetry thresholds have been proposed for supplemental oxygen use in infants with bronchiolitis, with the AAP guidelines suggesting its administration for oxygen saturation (SpO2) ≤90%. Most decisions are based on a single point measurement despite pulse oximetry being a dynamic process. It is unknown whether analysis of continuously measured SpO2 can more accurately identify clinically relevant desaturations compared to a single point in time.
Objective: We investigated the association between SpO2 measurements (at triage versus trend over time) and outcomes in infants with bronchiolitis, specifically: (1) respiratory progression or (2) severe bronchiolitis.
Design/Methods: In this ongoing prospective cohort study, we enrolled infants ≤90 days old presenting with bronchiolitis to the emergency department (ED). Standardized patient histories and examinations were completed. SpO2 was measured continuously at 1 Hz using pulse oximetry and downloaded for analysis. SpO2 values were censored at 1 hour after ED arrival or when supplemental oxygen or respiratory support was initiated, whichever came first. We examined 1) triage SpO2 > or ≤90%, 2) percent time below different SpO2 thresholds (≤89%, ≤90%, ≤91%), and 3) frequency of sustained desaturations (consecutive SpO2 values below defined threshold for 5 or 10 seconds) to investigate the association between these exposures and outcomes. We defined respiratory progression as new use of respiratory support within 24 hours of ED arrival. Severe bronchiolitis was defined as development of apnea, or receipt of HFNC or CPAP (≥2 days), BIPAP, or invasive ventilation.
Results: From November 2021 to August 2024, 168 infants were enrolled. Of these, 97 had ≥15 minutes of continuous SpO2 data (median 2,256 values) and were analyzed. Sixty-six (68%) had no or mild respiratory distress on exam (Table 1). Over half developed respiratory progression (n=53, 55%) and/or severe bronchiolitis (n=50, 52%). Triage SpO2 was ≤90% in 5 (5%) infants and was not associated with respiratory progression or severe bronchiolitis. Median percentage of time spent with SpO2 ≤89%, ≤90%, and ≤91% was 1.4%, 2.0%, and 2.9%, respectively (Table 2). Percentage of time spent with desaturations was associated with respiratory progression (for all SpO2 thresholds) and with severe bronchiolitis (for ≤91%). Sustained desaturations were associated with both outcomes for all SpO2 thresholds (Table 3).
Conclusion(s): Analysis of continuously measured SpO2 over one hour provides a better measure of oxygen desaturations and may improve accuracy of SpO2 in determining bronchiolitis severity.
Table 1. Demographics, presenting illness, and physical exam findings of young infants with bronchiolitis presenting to the emergency department (n=97*)
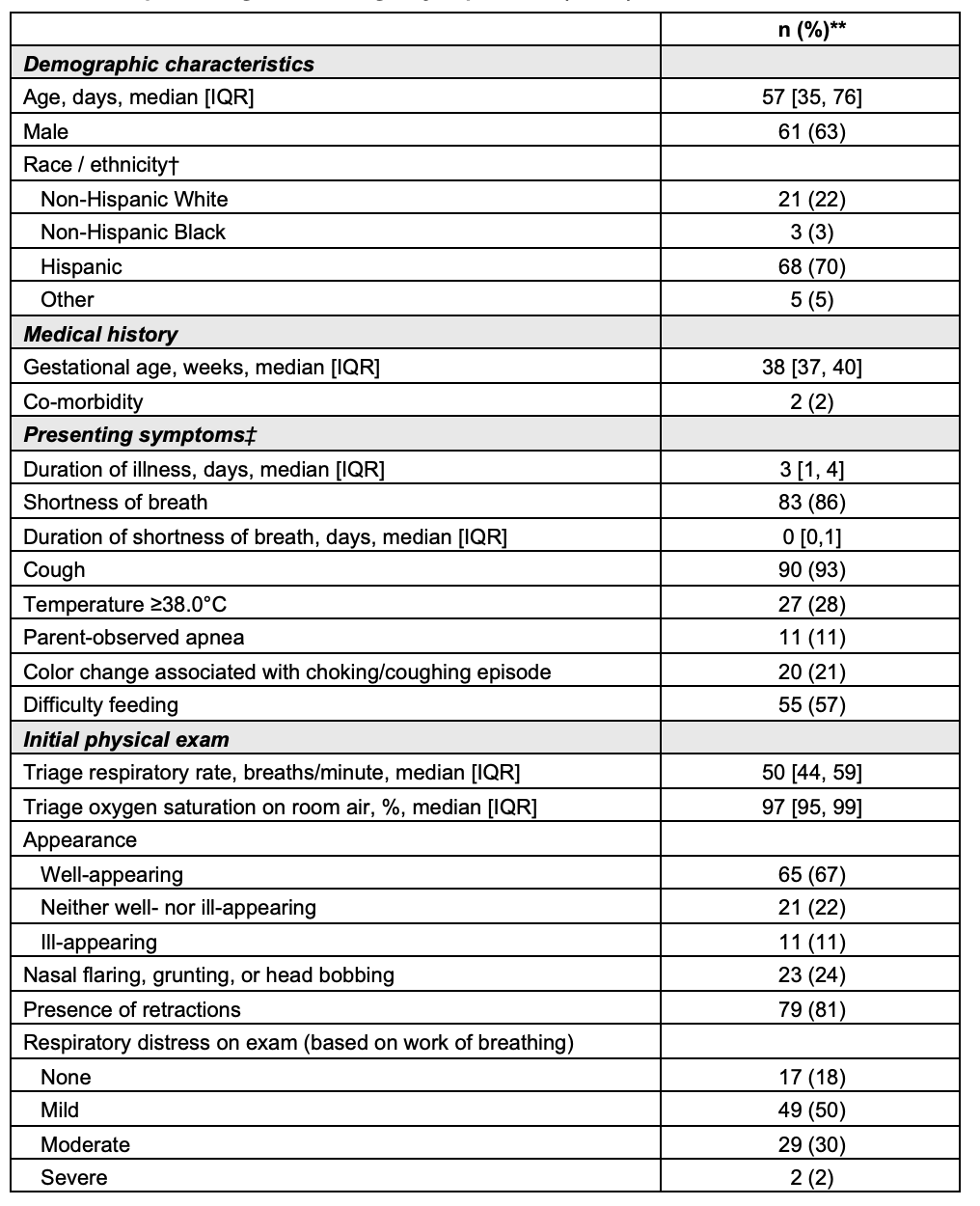 * Total number includes infants who had at least 15 minutes of continuously measured oxygen saturation data.
* Total number includes infants who had at least 15 minutes of continuously measured oxygen saturation data. ** All values are frequency (%) unless otherwise noted.
† Race and ethnicity for the infants were reported by their parents.
‡ With the exception of shortness of breath, presenting symptoms refer to symptoms present during the preceding 24 hours.
Table 2. Percentage of time spent with desaturations
.png) * Oxygen saturation thresholds were selected based on available bronchiolitis guidelines from USA (AAP, 2014: ≤90%), UK (NICE, 2015: ≤91%), Italy (2014: ≤89-91%), Spain (2010: ≤91%), and France (2013: ≤91%).
* Oxygen saturation thresholds were selected based on available bronchiolitis guidelines from USA (AAP, 2014: ≤90%), UK (NICE, 2015: ≤91%), Italy (2014: ≤89-91%), Spain (2010: ≤91%), and France (2013: ≤91%).** One-hour time frame was chosen as a feasible duration for monitoring in the emergency department.
† Respiratory progression was defined as new use of respiratory support within 24 hours of ED arrival. Respiratory support includes continuous or bilevel positive airway pressure, high-flow nasal cannula, and intubation for invasive mechanical ventilation.
‡ Severe bronchiolitis was defined as meeting any of the following: apnea resulting in initiation of respiratory support; use of continuous (≥2 days) or bilevel (any duration) positive airway pressure; use of high-flow nasal cannula (≥2 days); intubation for invasive mechanical ventilation.
Table 3. Frequency of sustained desaturations
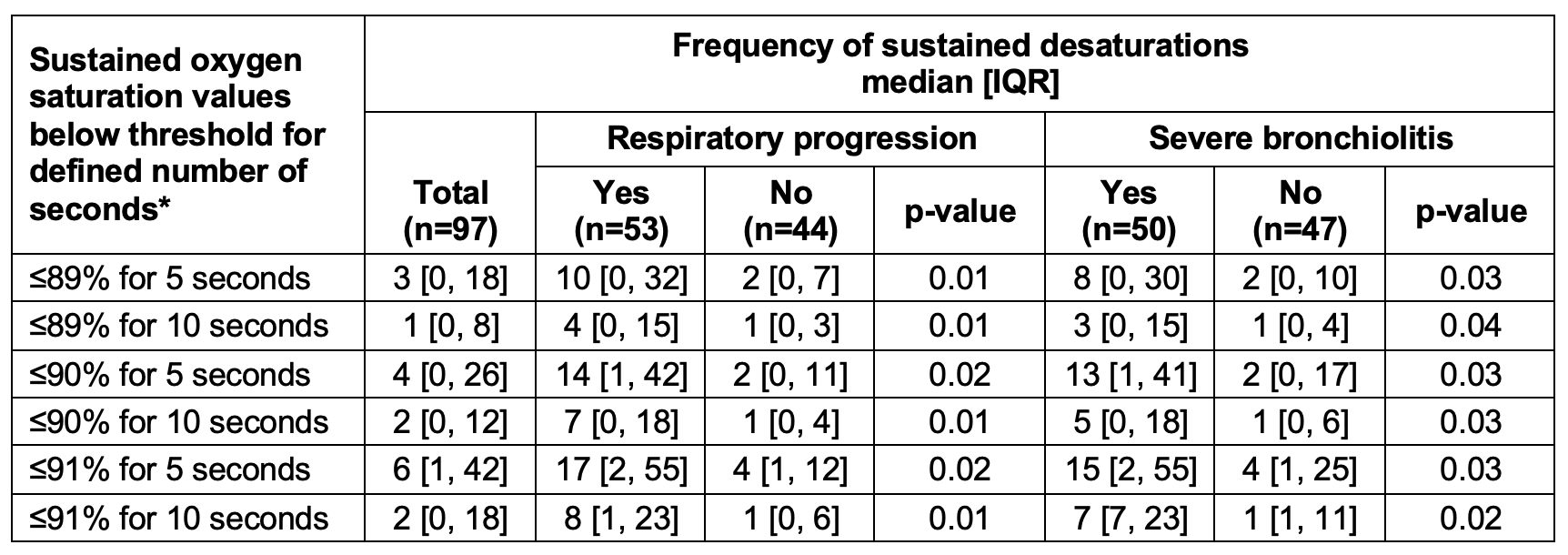 * Sustained desaturation was defined as consecutive desaturations lasting five or ten seconds. These consecutive desaturations were selected to capture true desaturations, minimizing the likelihood of artifacts or measurement errors. To account for differences in the duration of SpO2 data available for each patient, frequency of sustained desaturations was normalized.
* Sustained desaturation was defined as consecutive desaturations lasting five or ten seconds. These consecutive desaturations were selected to capture true desaturations, minimizing the likelihood of artifacts or measurement errors. To account for differences in the duration of SpO2 data available for each patient, frequency of sustained desaturations was normalized. Table 1. Demographics, presenting illness, and physical exam findings of young infants with bronchiolitis presenting to the emergency department (n=97*)
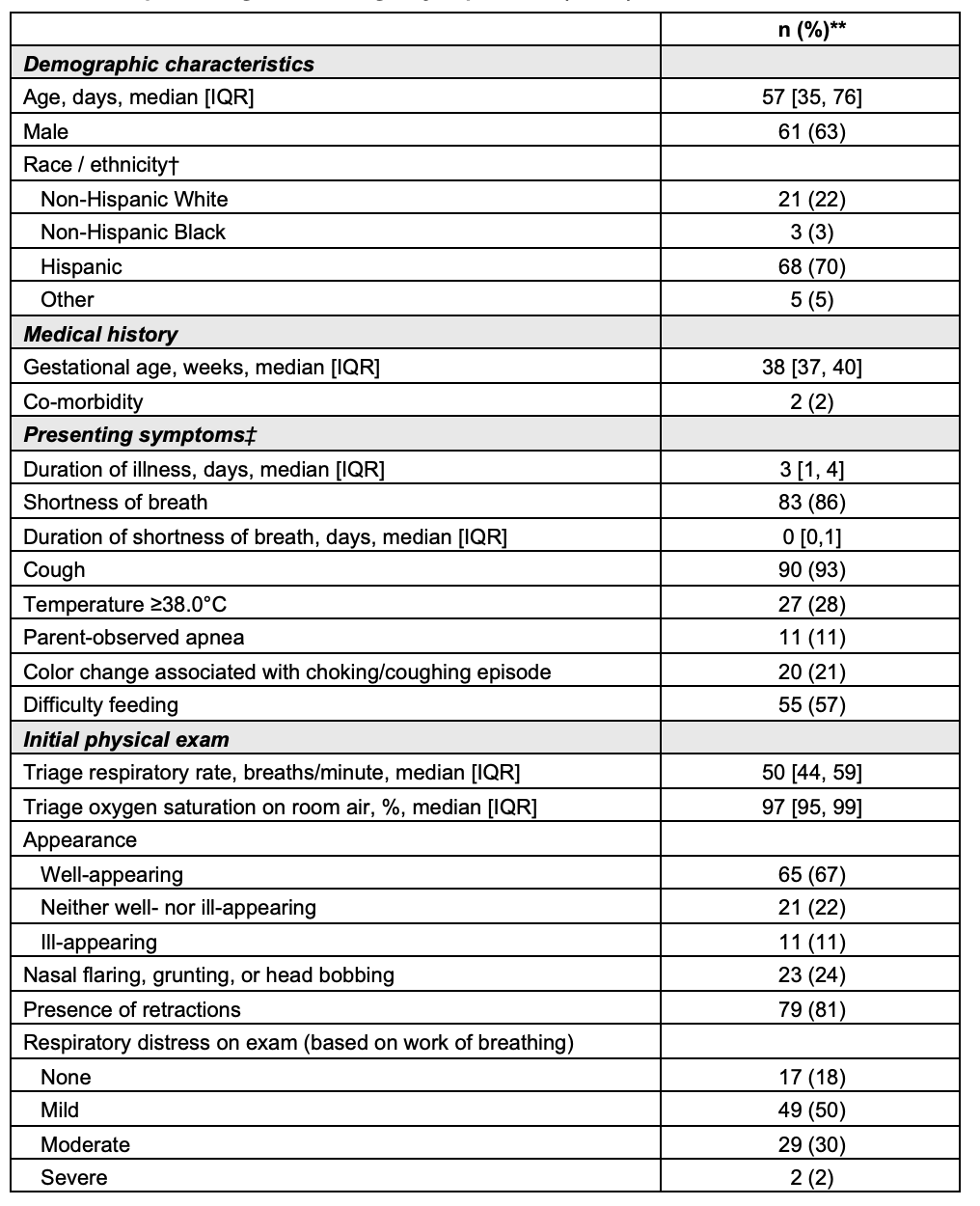 * Total number includes infants who had at least 15 minutes of continuously measured oxygen saturation data.
* Total number includes infants who had at least 15 minutes of continuously measured oxygen saturation data. ** All values are frequency (%) unless otherwise noted.
† Race and ethnicity for the infants were reported by their parents.
‡ With the exception of shortness of breath, presenting symptoms refer to symptoms present during the preceding 24 hours.
Table 2. Percentage of time spent with desaturations
.png) * Oxygen saturation thresholds were selected based on available bronchiolitis guidelines from USA (AAP, 2014: ≤90%), UK (NICE, 2015: ≤91%), Italy (2014: ≤89-91%), Spain (2010: ≤91%), and France (2013: ≤91%).
* Oxygen saturation thresholds were selected based on available bronchiolitis guidelines from USA (AAP, 2014: ≤90%), UK (NICE, 2015: ≤91%), Italy (2014: ≤89-91%), Spain (2010: ≤91%), and France (2013: ≤91%).** One-hour time frame was chosen as a feasible duration for monitoring in the emergency department.
† Respiratory progression was defined as new use of respiratory support within 24 hours of ED arrival. Respiratory support includes continuous or bilevel positive airway pressure, high-flow nasal cannula, and intubation for invasive mechanical ventilation.
‡ Severe bronchiolitis was defined as meeting any of the following: apnea resulting in initiation of respiratory support; use of continuous (≥2 days) or bilevel (any duration) positive airway pressure; use of high-flow nasal cannula (≥2 days); intubation for invasive mechanical ventilation.
Table 3. Frequency of sustained desaturations
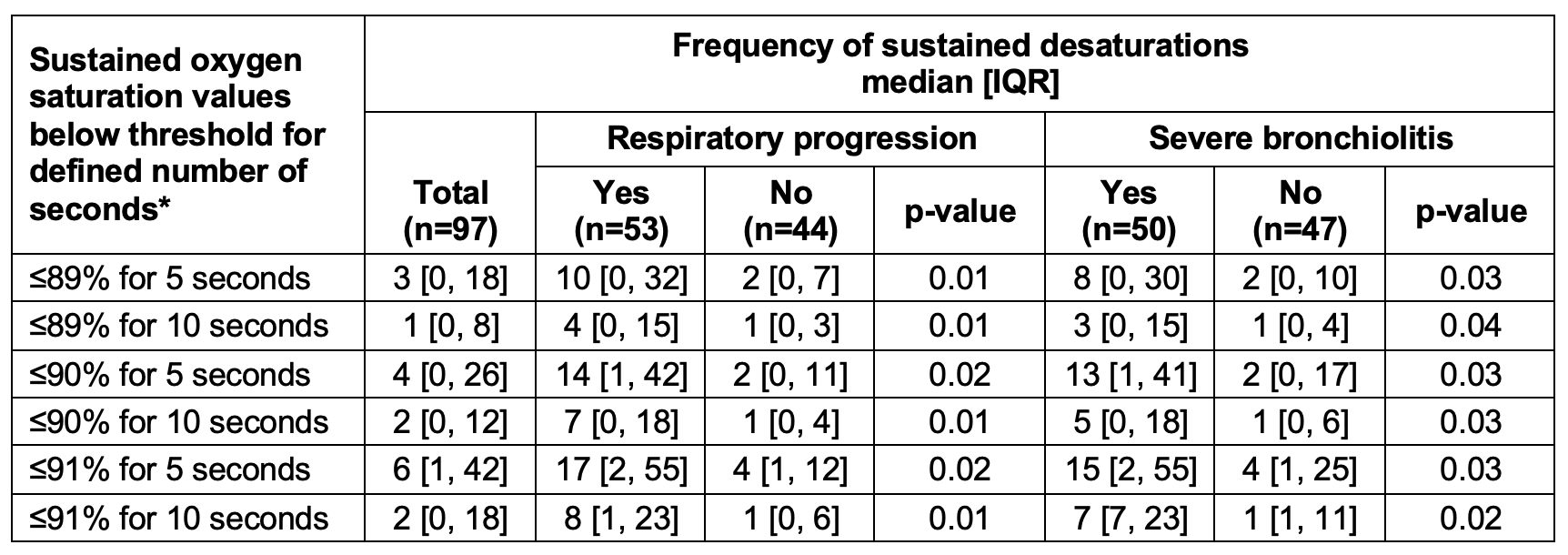 * Sustained desaturation was defined as consecutive desaturations lasting five or ten seconds. These consecutive desaturations were selected to capture true desaturations, minimizing the likelihood of artifacts or measurement errors. To account for differences in the duration of SpO2 data available for each patient, frequency of sustained desaturations was normalized.
* Sustained desaturation was defined as consecutive desaturations lasting five or ten seconds. These consecutive desaturations were selected to capture true desaturations, minimizing the likelihood of artifacts or measurement errors. To account for differences in the duration of SpO2 data available for each patient, frequency of sustained desaturations was normalized. 
