General Pediatrics 3
Session: General Pediatrics 3
219 - Healthcare Experience of Immigrant Families with Children with Special Healthcare Needs: A Focus on Medical Home Components, Family-Centered Care, and Care Coordination
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 219.5120
RASHEDAT OSHODI, University of Minnesota Medical School, Eden Prairie, MN, United States; Rebecca Freese, University of Minnesota, Minneapolis, MN, United States; Iris W. Borowsky, University of Minnesota Medical School, Minneapolis, MN, United States

Rashedat Oshodi, MD (she/her/hers)
Pediatric Physician
University of Minnesota Medical School
Eden Prairie, Minnesota, United States
Presenting Author(s)
Background: Children with special health care needs (CSHCN) in immigrant families face health disparities and risks for serious morbidity. They may receive lower quality care due to barriers accessing care and engaging in the health care and social systems.
Objective: We assessed quality of health care for CSHCN in US immigrant families, including receipt of components of the medical home, family-centered care (FCC), and care coordination (CC).
Design/Methods: Using the 2020-2022 National Survey of Children’s Health (NSCH), we assessed characteristics of CSHCN by immigrant family type: foreign-born child with no parent in the household born in the US (foreign-born child), US born child with at least one foreign-born parent in the household (foreign-born parent), all parents in the household born in the US (US-born parents)
We used logistic regression to compare parents' reported experience with having a medical home, family centered care, and care coordination by immigrant family type controlling for confounding variables such as age, sex, primary language, family structure, insurance status and income level.
Results: Families with a foreign-born child were less likely than families with a foreign-born parent or US born parents to have a medical home or usual source of sick care and receive family-centered care (FCC). More families with a foreign-born child were uninsured (13%) compared to the other immigrant family groups (foreign-born parent 3.7%; US-born parents 3.6%).
In adjusted models, families with a foreign-born parent had higher odds of receiving family-centered care (FCC) (AOR 0.93, CI 0.73 – 1.19) compared to families with a foreign-born child (AOR 0.60, CI 0.38 – 0.95). Additionally, families with a foreign-born child were less likely than those with either foreign-born or US-born parents to experience key FCC components, such as doctors listening, showing cultural sensitivity, or collaborating in care.
For all families, lacking insurance was significantly associated with non-receipt of all FCC components and medical home components except for care coordination.
Conclusion(s): Disparities we found in medical homes and FCC among immigrant families with CSHCN likely reflect unique access challenges requiring further study. Community outreach through culturally competent, trusted sources to educate families on healthcare rights and navigation could help, in addition to expanding access to health insurance through affordable private insurance and easing eligibility for public federal programs to reduce access gaps.
Characteristics of Sample by Immigrant family type.
.png)
Unadjusted and Adjusted odds of medical home and components.
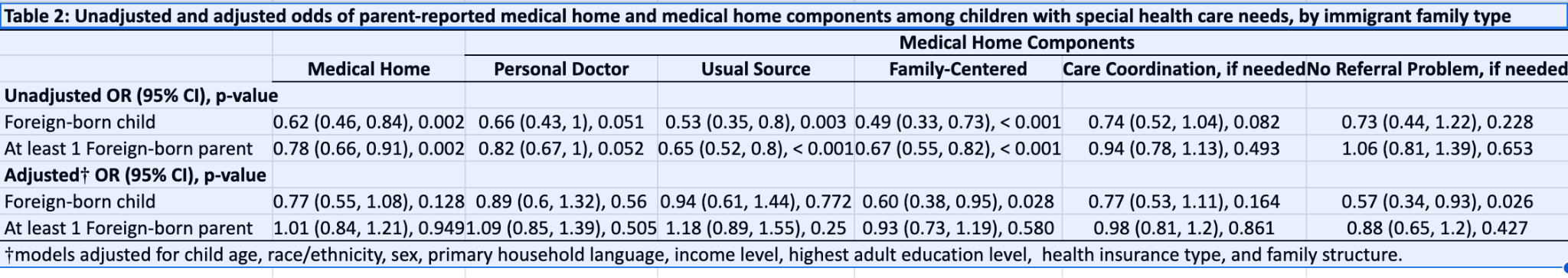 The reference group is US-born parents.
The reference group is US-born parents.Unadjusted and adjusted odds of family centered care components.
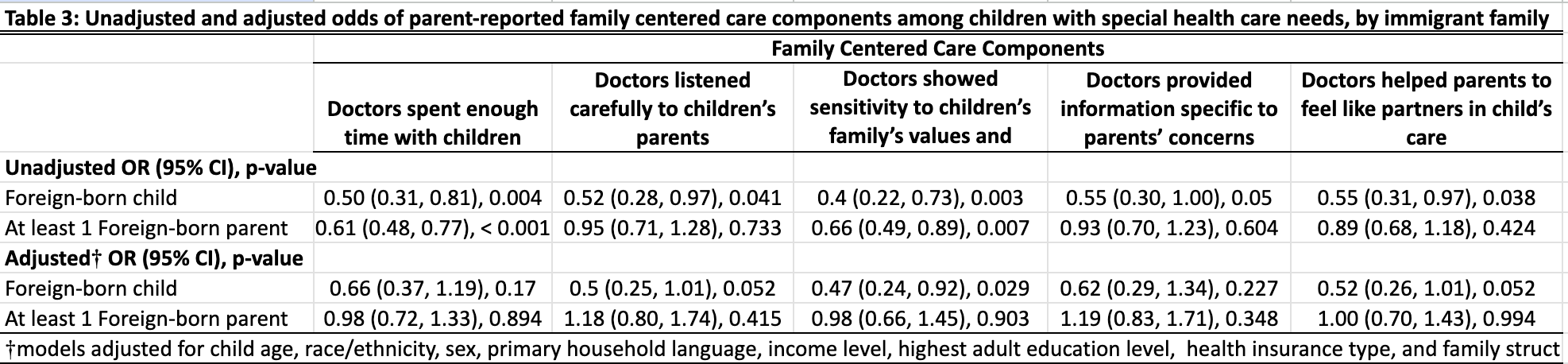 The reference group is US-born parents.
The reference group is US-born parents.Characteristics of Sample by Immigrant family type.
.png)
Unadjusted and Adjusted odds of medical home and components.
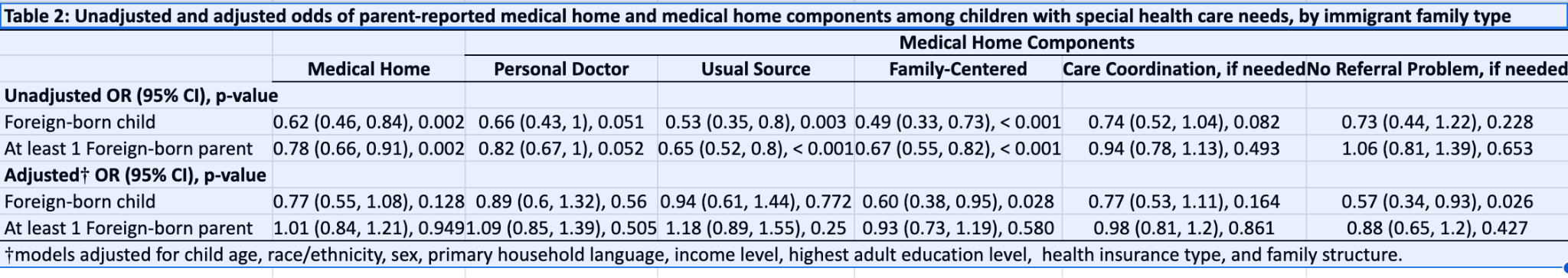 The reference group is US-born parents.
The reference group is US-born parents.Unadjusted and adjusted odds of family centered care components.
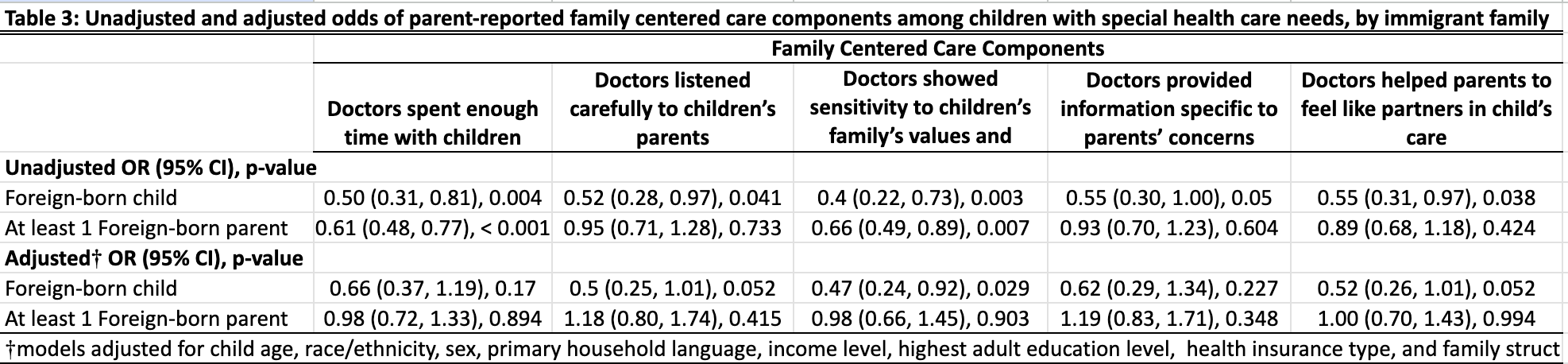 The reference group is US-born parents.
The reference group is US-born parents.
