Medical Education 10: Outpatient and primary care pediatrics
Session: Medical Education 10: Outpatient and primary care pediatrics
203 - Impact of An Inpatient Community Pediatrics Curriculum at One Year
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 203.5111
Ria Gupta, Johns Hopkins University School of Medicine, Katy, TX, United States; C. Nicholas Cuneo, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Amy Davis, Johns Hopkins School of Medicine, Baltimore, MD, United States; Eric Balighian, Johns Hopkins University School of Medicine, Baltimore, MD, United States; Emily Murphy, Johns Hopkins University School of Medicine, Baltimore, MD, United States

Ria Gupta, BS (she/her/hers)
Medical Student
Johns Hopkins University School of Medicine
Katy, Texas, United States
Presenting Author(s)
Background: The Accreditation Counsel for Graduate Medical Education (ACGME) requires ambulatory experiences in community pediatrics with successful frameworks for implementing ambulatory experiences (Hoffman 2017), however, it is less clear how to successfully teach community pediatrics skills in the inpatient setting.
Objective: We designed a longitudinal inpatient community pediatrics curriculum (CPC) for pediatric residents and aimed to assess the preliminary feasibility and impact of the curriculum.
Design/Methods: Pediatric residents participate in inpatient rotations and the CPC longitudinally at the residency program’s separately affiliated hospital which serves as their community site. The CPC consists of didactics, engagement activities at community-based organizations, a bus tour led by a community member, and a previously published home visit curriculum (Balighian 2020). To assess the CPC, we designed a pre- and post-rotation survey assessing resident characteristics, curriculum participation, confidence in community pediatrics activities on a 5-point Likert scale, and knowledge of SDoH resources. Residents complete the surveys during each rotation. We performed preliminary analysis after approximately 1 year of data collection (June 2022 to October 2023). We performed descriptive statistical analysis and compared resident survey outcomes pre- and post-curriculum with paired T-test and Chi-square analysis. The study was approved by the Institutional Review Board.
Results: Seventy-seven residents participated in the CPC during the preliminary study period. Fifty-six residents completed the pre-survey (72.7%) and 38 (49.4%) completed the post-survey. Residents who completed the survey were primarily categorical pediatrics residents in PGY-1, female, and non-Hispanic white (Table 1). Participation in CPC activities was high for all activities except patient home visit (6 residents, 15.8%). Post-CPC, residents reported increased confidence in multiple skills related to community pediatrics and were more likely to be able to name specific resources for SDoH needs across multiple domains (Table 2).
Conclusion(s): Our preliminary findings demonstrate feasibility of an integrated inpatient CPC, although further resources may be required to ensure consistent home visit participation. The CPC does not require additional educational units within residency programming while still resulting in significant affective and knowledge change in residents. Next steps include final survey data analysis, qualitative analysis of resident experiences, and evaluation of patient-level outcomes.
Table 1: Characteristics of residents participating in Community Pediatrics Curriculum
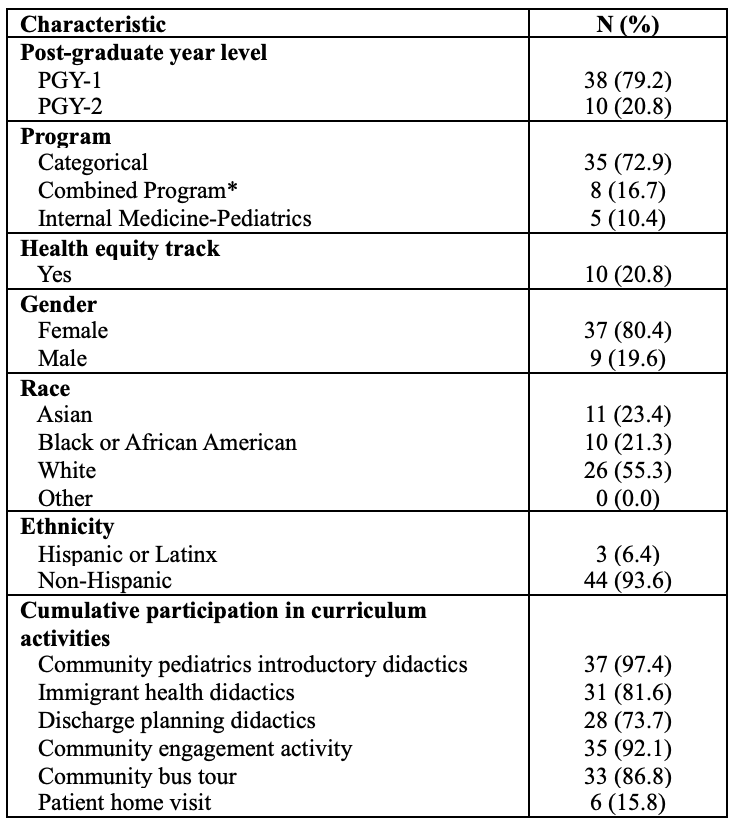 Abbrev: PGY, postgraduate year
Abbrev: PGY, postgraduate year*Pediatric Neurology, Pediatric Anesthesia, or Pediatric Genetics
Table 2: Change in resident confidence and knowledge in social determinants of health resources, pre- and post-curriculum
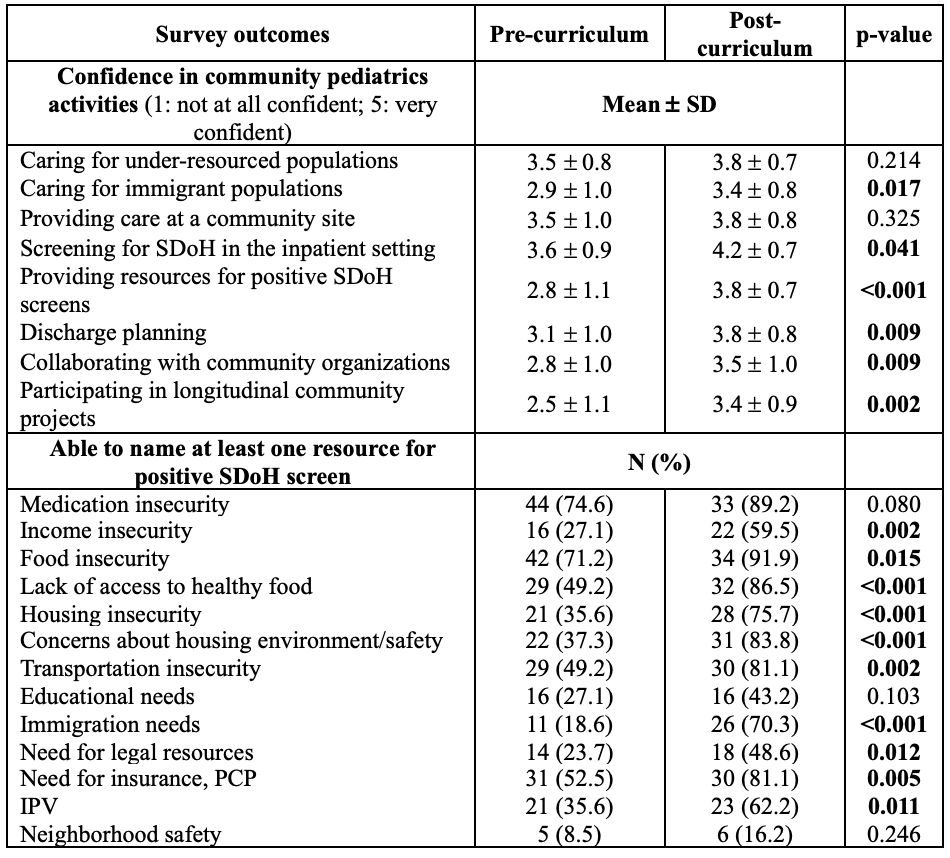 Abbrev: SDoH, social determinants of health; PCP, primary care physician; IPV, interpersonal violence
Abbrev: SDoH, social determinants of health; PCP, primary care physician; IPV, interpersonal violenceTable 1: Characteristics of residents participating in Community Pediatrics Curriculum
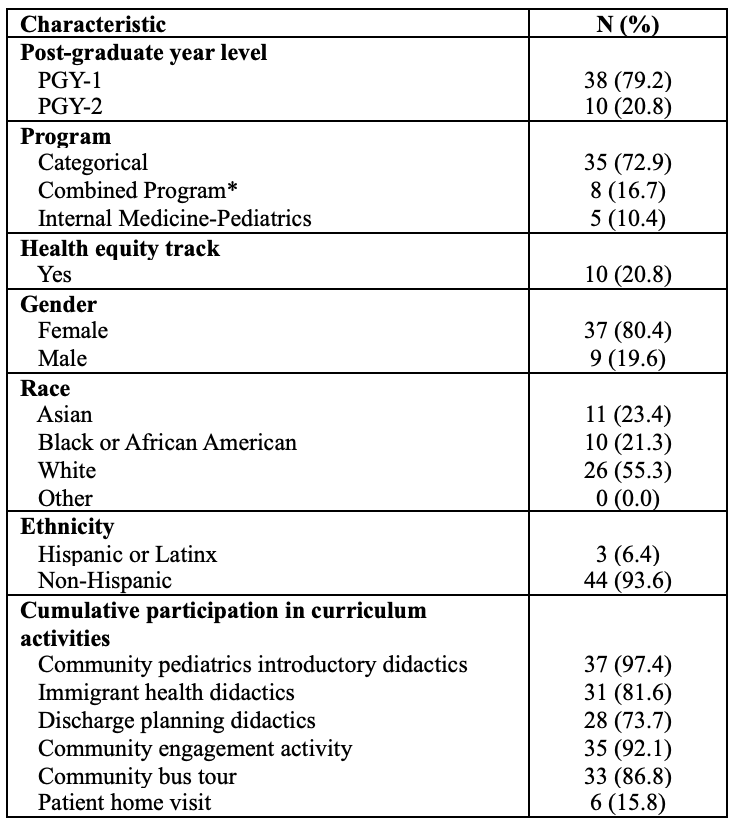 Abbrev: PGY, postgraduate year
Abbrev: PGY, postgraduate year*Pediatric Neurology, Pediatric Anesthesia, or Pediatric Genetics
Table 2: Change in resident confidence and knowledge in social determinants of health resources, pre- and post-curriculum
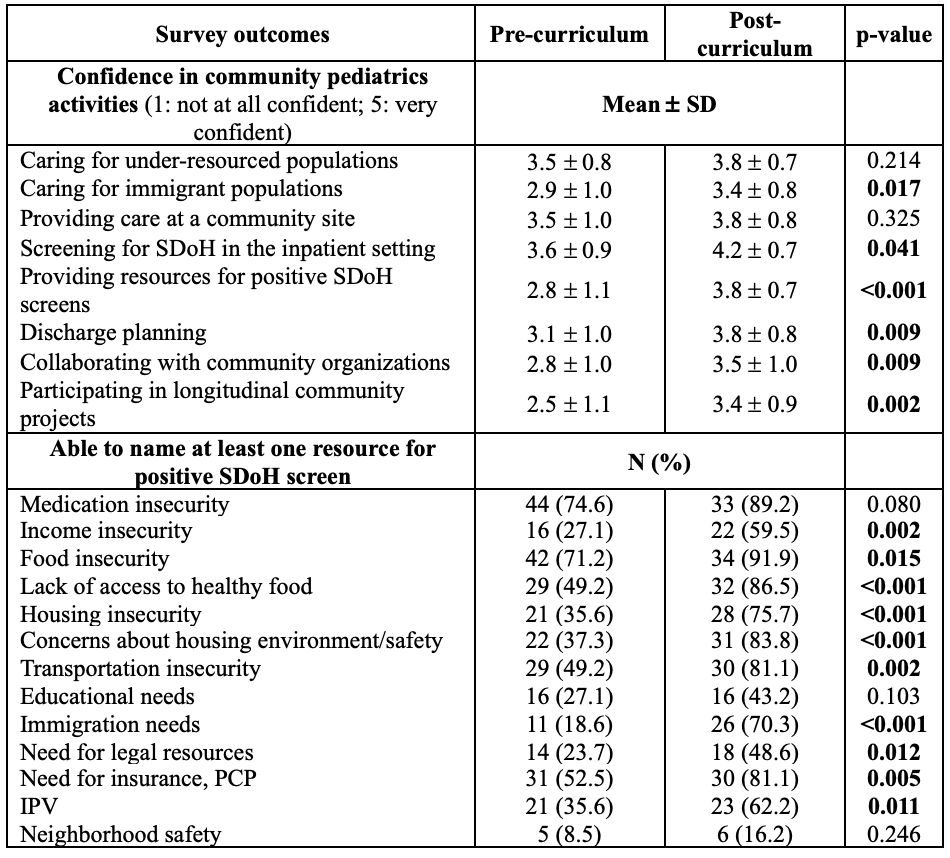 Abbrev: SDoH, social determinants of health; PCP, primary care physician; IPV, interpersonal violence
Abbrev: SDoH, social determinants of health; PCP, primary care physician; IPV, interpersonal violence
