Hospital Medicine 3: Systems/Population-based Research
Session: Hospital Medicine 3: Systems/Population-based Research
144 - Identification of Potentially Avoidable Pediatric Transfers from Rural and Indian Health Service Emergency Departments
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 144.5265
Andrew Steinfeldt, Phoenix Children's Hospital, Phoenix, AZ, United States; Cherisse Mecham, Phoenix Children's Hospital, Phoenix, AZ, United States; Kyle P. Craddock, Phoenix Children’s Hospital, Tucson, AZ, United States; Isrealia Jado, University of Arizona College of Medicine - Phoenix, Phoenix, AZ, United States; Karen Yeager, Phoenix Children's, Phoenix, AZ, United States; Hamy Temkit, Phoenix Children's Hospital, Phoenix, AZ, United States; Fiona Pirrocco, Children’s Hospital of Philadelphia, Philadelphia, PA, United States
- AS
Andrew Steinfeldt, MD (he/him/his)
PEM Fellow
Phoenix Children's Hospital
Phoenix, Arizona, United States
Presenting Author(s)
Background: In Arizona, approximately 68% of American Indian/Alaska Native peoples reside in rural areas which are often on or near their tribal homelands. Pediatric patients are transferred to larger health facilities more frequently than adults, which may be exacerbated in Indian Health Service (IHS) emergency departments (EDs) due to resource limitations. The National Pediatric Readiness Project (NPRP) seeks to enhance pediatric capabilities and includes a survey to assess pediatric readiness.
Objective: This study evaluates the rate of potentially avoidable transfers (PATs) from IHS EDs to a tertiary children’s hospital ED and examines the correlation between PAT rates and 2021 NPRP pediatric readiness scores.
Design/Methods: This IRB-approved, single-center, retrospective chart review analyzed transfer data from a tertiary children’s hospital ED from January 2017 to December 2020, identifying PATs through electronic health records. A PAT was defined as a patient discharged within 24 hours without advanced procedures, in-person subspecialist consultations, or advanced imaging. Pediatric readiness scores were obtained from the EMSC data center. Data were summarized using descriptive statistics, and Pearson correlation was used to assess the relationship between PAT rates and readiness scores.
Results: Among 2,266 patient encounters from 19 facilities, the average PAT rate was 34.2%, showing statistical significance across all four years. While PAT rates trended downwards over time, the need for in-person subspecialist consultations increased. No significant correlation was found between PAT rates and readiness scores, but facilities engaged in the EMSC readiness survey showed significantly lower PAT rates than those who didn’t.
Conclusion(s): Over a third of ED-to-ED transfers were potentially avoidable, with no correlation to pediatric readiness scores. However, facilities actively participating in the readiness survey demonstrated decreased PAT rates, suggesting that improving pediatric readiness awareness may enhance care. The rising trend of transfers requiring in-person subspecialist consultations highlights issues in pediatric care regionalization and underscores the need for better access to subspecialists. Further research is essential to understand the factors driving PATs, which could inform future resource allocation and outreach efforts.
Potentially Avoidable Transfer Rates by Year
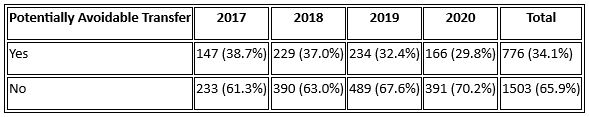 Note: The 95% Confidence interval (CI) for potential avoidable transfer by year and overall: 2017(33.8%,43.6%), 2018(33.5%,41.2%), 2019(29.1%,35.9%), 2020(26.2%,33.8%), overall (32.3%, 36.2%). P<0.01
Note: The 95% Confidence interval (CI) for potential avoidable transfer by year and overall: 2017(33.8%,43.6%), 2018(33.5%,41.2%), 2019(29.1%,35.9%), 2020(26.2%,33.8%), overall (32.3%, 36.2%). P<0.01 
