Hospital Medicine 5: Clinical
Session: Hospital Medicine 5: Clinical
528 - Factors Associated with 7-day Hospital Readmission After Tracheostomy Associated Respiratory Infection: A Multicenter Retrospective Cohort Study
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 528.4878
Angela Pluguez, USF Health Morsani College of Medicine, Saint Petersburg, FL, United States; Nicholas A. Jabre, Johns Hopkins All Children's Hospital, Saint Petersburg, FL, United States; Joana Machry, Johns Hopkins All Children's Hospital, SAINT PETERSBURG, FL, United States; Julia Krzyzewski, Johns Hopkins All Children's Hospital, St. Petersburg, FL, United States; Beatriz Teppa Sanchez, Johns Hopkins All Children's Hospital, SAINT PETERSBURG, FL, United States; John Morrison, Johns Hopkins All Children's Hospital, Saint Petersburg, FL, United States

Angela Pluguez, DO (she/her/hers)
Resident Physician
USF Health Morsani College of Medicine
Saint Petersburg, Florida, United States
Presenting Author(s)
Background: Children with tracheostomy are frequently readmitted after inpatient treatment for tracheostomy-associated respiratory infections (TARIs). Several risk factors have been identified for readmission within 30 days of discharge. However, this timeframe may reflect newly acquired conditions and not opportunities for improving inpatient care.
Objective: Describe prevalence of and explore factors associated with 7-day hospital readmission among patients treated for TARI.
Design/Methods: We conducted a multicenter retrospective cohort study using the Pediatric Health Information System (PHIS) database. De-identified data for inpatient encounters from 48 freestanding children’s hospitals were obtained for children with tracheostomy 0-21 years of age, hospitalized with principal diagnoses consistent with TARI (e.g. pneumonia, tracheitis) between 1/1/2017 to 1/31/2024. Encounters with mortality or planned readmissions were excluded. Our primary outcome was all-cause hospital readmission within 7 days of discharge. Demographic factors, diagnostic evaluation, and medical care received during the index hospitalization were extracted from PHIS and compared between patients with and without readmission. We explored the associations between demographic, diagnostic evaluation, and inpatient treatment factors and our primary outcome using multivariable logistic regression.
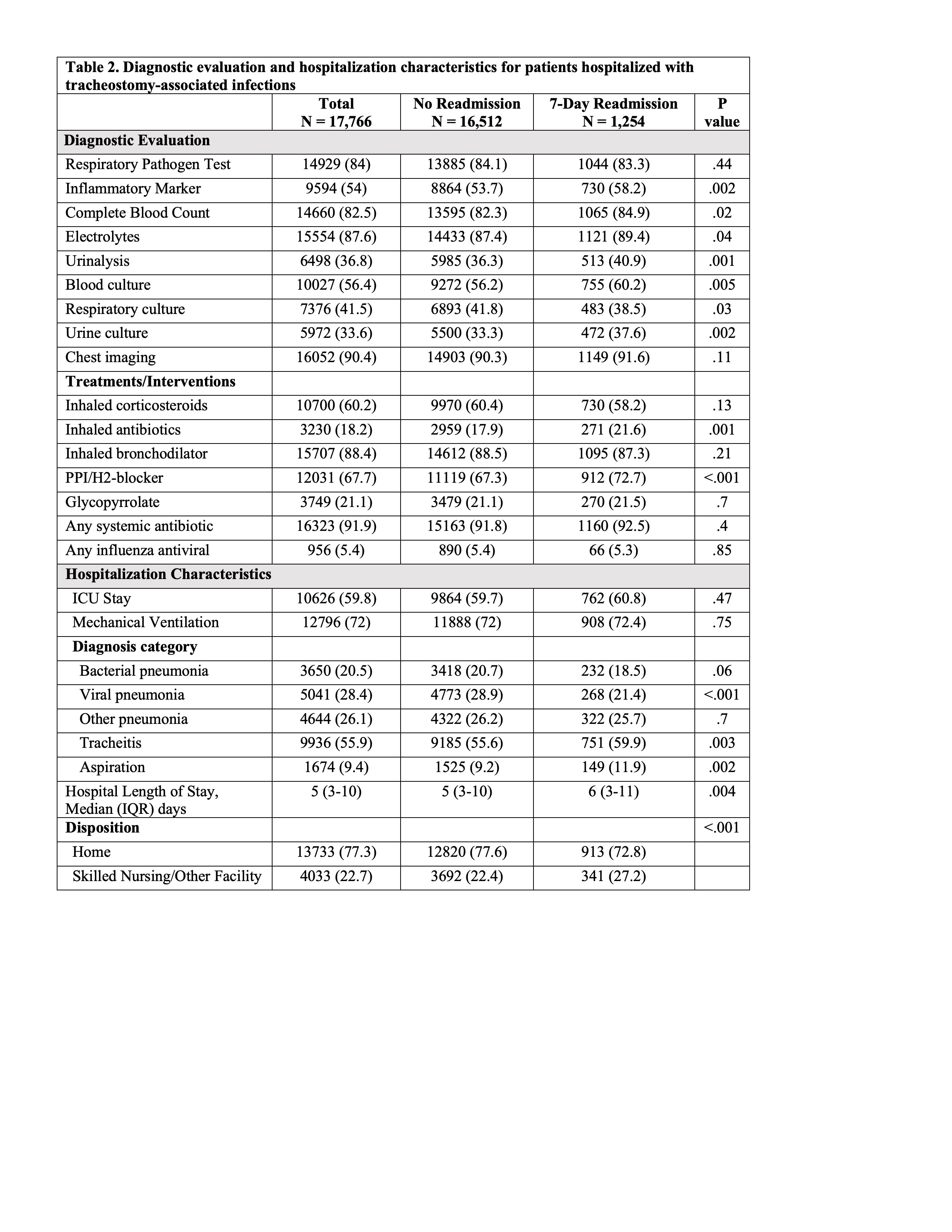
Results: Readmission occurred in 1,254/17,766 (7.1%) of TARI encounters, ranging from 0-11.3% across sites (Fig. A). Demographic, diagnostic, and hospital course data are summarized in Tables 1 and 2. The median (IQR) age at admission was 5 (2, 11) years and 83% of encounters had ≥3 chronic complex conditions. Respiratory pathogen (84%) and inflammatory marker (54%) testing were frequently obtained (Fig. B). Systemic antibiotics were prescribed in 92% of encounters (Fig. C). Patients with a readmission had a longer median [IQR] length of stay (6 [3-11] vs. 5[3-10]; p=.008). In multivariable analysis (Fig. D), older age, receipt of inhaled corticosteroids, and viral TARI diagnosis were associated with reduced odds of readmission. Inflammatory marker testing and antacid prescription were associated with increased odds of readmission.
Conclusion(s): Nearly 1 in 14 TARI hospitalizations resulted in 7-day readmission. Patients with viral TARIs may be at reduced odds of readmission due to the self-limiting nature of viral illness. Antibiotic and anti-inflammatory treatment was common in TARI encounters with variable effects on readmission. Future research to optimize pre-discharge care, including the role of specific pharmacological interventions is warranted.
Figure
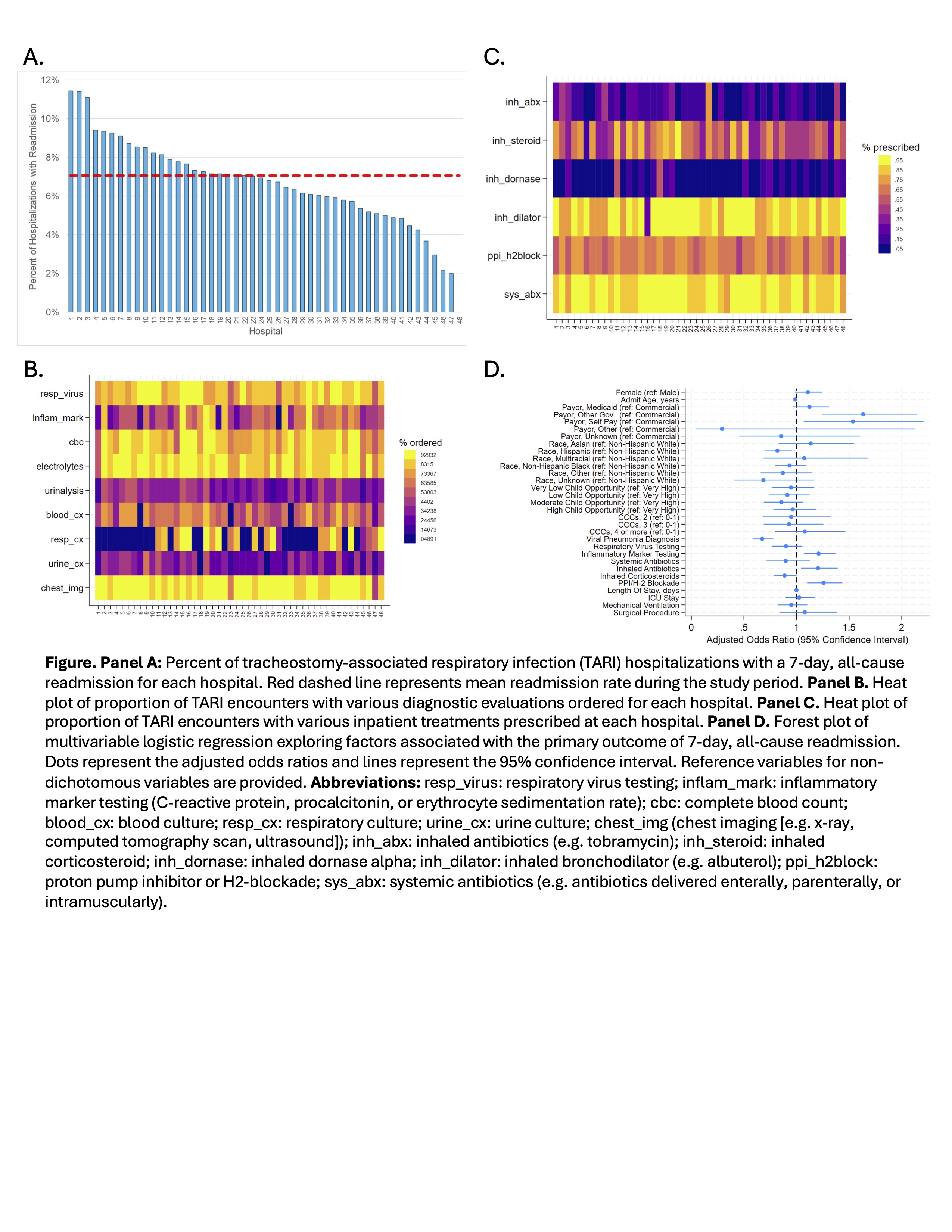
Table 1
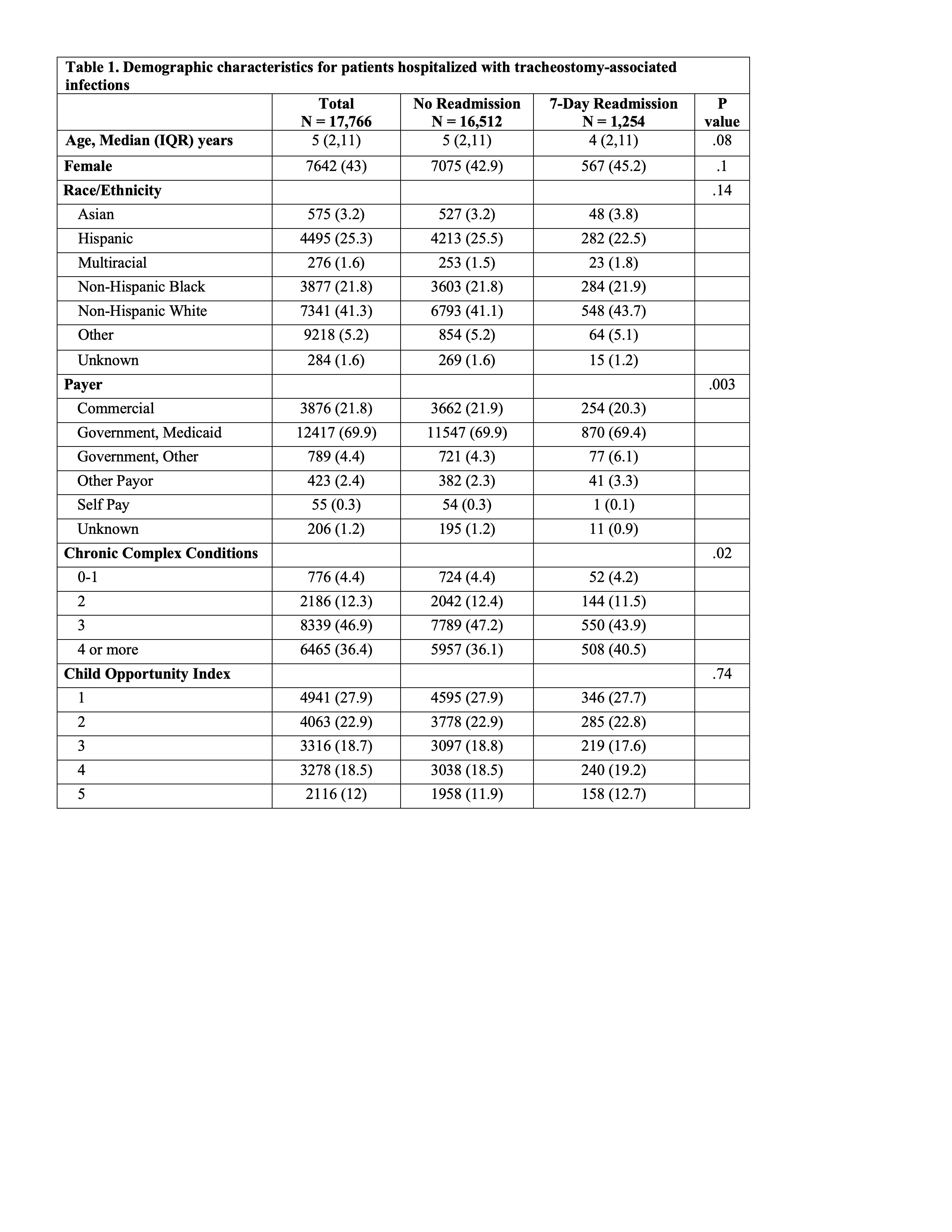
Table 2