Health Equity/Social Determinants of Health 5
Session: Health Equity/Social Determinants of Health 5
708 - Achieving Equity in Early Childhood Vaccinations for Native Hawaiians and Other Pacific Islanders
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 708.3726
Jacob J. Fitisemanu, Intermountain Health, West Valley City, UT, United States; Tim Fowles, Intermountain Health, Salem, UT, United States; Sarah Abdelaziz, Intermountain Health, Salt Lake City, UT, United States; Ashley Krueger, Intermountain Health, Salt Lake City, UT, United States; Justin B. Poll, Intermountain Health, South Weber, UT, United States; Carolyn Reynolds, Intermountain Healthcare, Salt Lake City, UT, United States; Carole H. Stipelman, University of Utah School of Medicine, Salt Lake City, UT, United States; Roy N. Davis, Intermountain Children's Health, Murray, UT, United States

Jacob J. Fitisemanu, Jr., MPH (he/him/his)
Program Manager
Intermountain Health
West Valley City, Utah, United States
Presenting Author(s)
Background: Early childhood vaccinations (ECV) are critical to protect children and their communities. Intermountain Health (IH) provides healthcare in 6 states for > 42,000 children aged 2 y annually. A disparity in vaccine completion at 2 y was noted, with lower frequency in children with parents who self-identified as Native Hawaiian and Other Pacific Islanders. (NHPI) (Figure 1). This may stem from inequities in access to care, mismatches between cultural preferences and the healthcare system, and views about vaccination and well-child visits (WCV). IH partnered with the Utah Pacific Islander Health Coalition (UPIHC) to address this disparity.
Objective: The objective of this nonintervention study was to develop quality measures and corrective actions for a multistate initiative to improve NHPI ECV completion.
Design/Methods: A key driver diagram was created to identify factors impacting ECV frequency (Figure 2). In children who reached age 2 y from January 2020 to December 2023, vaccination frequency and the effect of attending the 18-mo WCV were compared in NHPI vs non-NHPI children using χ2-test (Table). Interviews with NHPI families (12 total: 3 with fully vaccinated and 9 with partially or completely unvaccinated children) were performed. Corrective actions were designed from results of quantitative and qualitative analyses and tested for feasibility.
Results: Vaccination frequency was lower in children from NHPI v. non-NHPI families (Table 1). Attending the 18-mo WCV was associated with a higher proportion of fully vaccinated NHPI and non-NHPI children. Vaccines requiring a 4th dose at ≥ 12 mo were least likely to be completed by 2 y. Barriers identified in interviews included: travel to islands, childcare by elders, WCV may not be a common part of healthcare culture, access to care, beliefs about vaccine timing. Corrective actions tested for feasibility included: (1) outreach to NHPI families by specially-trained care managers to schedule overdue WCVs, emphasizing the 18-mo WCV, (2) UPIHC-led NHPI vaccine-oriented events with community health workers to help schedule WCV, and (3) UPIHC use of existing person-to-person and digital communication channels within the NHPI community (known in the community as Coconut Wireless) to promote vaccine confidence.
Conclusion(s): Collaboration between UPIHC and IH enabled development of community-informed interventions to improve vaccine equity for NHPI children. The interventions may be implemented using plan-do-study-act cycles with outcomes shared with the community by UPIHC.
Figure 1. Intermountain Health vaccine compliance dashboard revealing vaccine inequity
.png) Legend, Figure 1: Run chart of combination 7 completion by all children vs. Native Hawaiian and Other Pacific Islanders from January 2020 through July 2024. This group of 9 vaccines to measure early childhood vaccine compliance is named Combination 7 by the Advisory Committee on Immunization Practices, a committee within the United States Centers for Disease Control and Prevention. Inclusion criteria: any child with a primary care visit in the time period.
Legend, Figure 1: Run chart of combination 7 completion by all children vs. Native Hawaiian and Other Pacific Islanders from January 2020 through July 2024. This group of 9 vaccines to measure early childhood vaccine compliance is named Combination 7 by the Advisory Committee on Immunization Practices, a committee within the United States Centers for Disease Control and Prevention. Inclusion criteria: any child with a primary care visit in the time period.Figure 2. Driver diagram of factors affecting early childhood vaccination
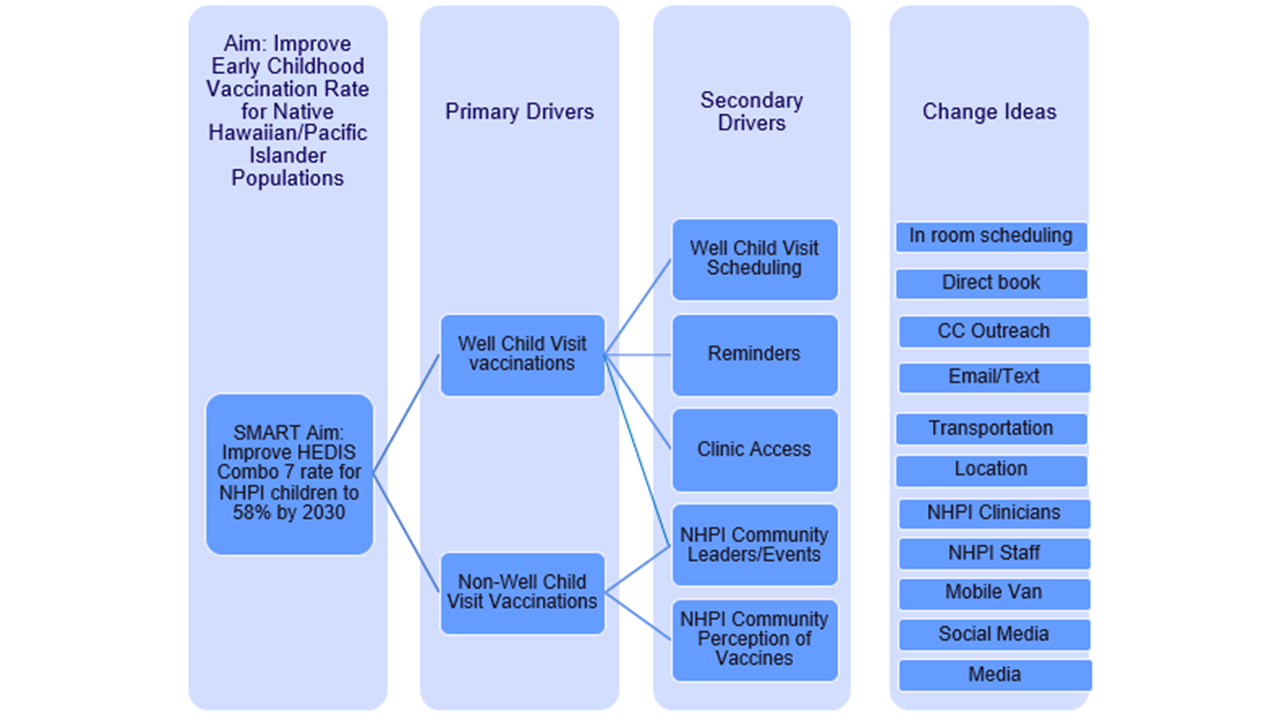 Abbreviations for Figure 2: SMART = Specific, Measurable, Achievable, Relevant, Time-Bound; NHPI=Native Hawaiian and Other Pacific Islanders; CC = Care Coordination
Abbreviations for Figure 2: SMART = Specific, Measurable, Achievable, Relevant, Time-Bound; NHPI=Native Hawaiian and Other Pacific Islanders; CC = Care CoordinationTable 1. Vaccination completion in children who reached age 2 years from January 2020 to December 2023 at Intermountain Health
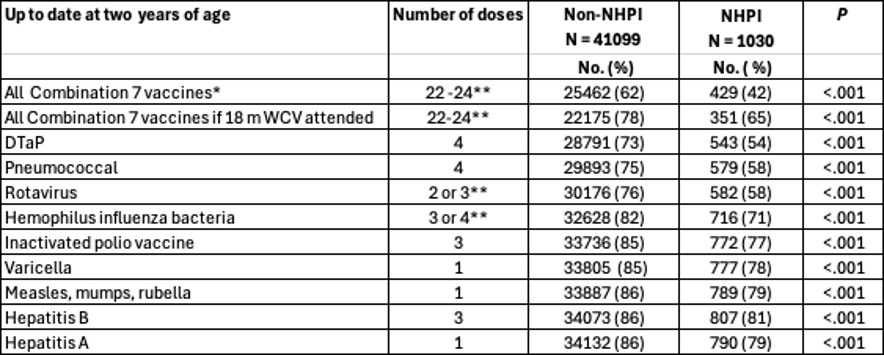 Legend, Table 1:
Legend, Table 1: Data reported as no. of children (%). Inclusion criteria: had well-child care, an Intermountain primary care, seen in system beyond 1 month of age.
*This group of 9 vaccines to measure early childhood vaccine compliance is named Combination 7 by the Advisory Committee on Immunization Practices, a committee within the United States Centers for Disease Control and Prevention
** Number of doses depends on vaccine brand used.
Abbreviations: DTaP, diphtheria, tetanus, and pertussis; NHPI, Native Hawaiian and Other Pacific Islanders.


