Emergency Medicine 7
Session: Emergency Medicine 7
092 - Clinical Outcomes of Children with Bronchiolitis Who Undergo High-Flow Nasal Cannula Utilization in the Emergency Department
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 92.4151
Andrea Rivera-Sepulveda, Nemours Children's Health, ORLANDO, FL, United States; Anushka Bhowal, University of Texas Southwestern Medical School, Dallas, TX, United States; Joel Hernandez, Nemours Children's Hospital, Orlando, FL, United States; Kiah Hill, Nemours Children's Hospital, Orlando, FL, United States; Kathryn Blake, Nemours Children's Health, Jacksonville, FL, United States; Matthew M. Davis, Nemours Children's Hospital, Wilmington, DE, United States

Anushka Bhowal, Doctor of Medicine (she/her/hers)
Pediatric Hospital Medicine - Clinical Fellow
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: In 2021, our independent children's healthcare system created a clinical pathway (CP) for the emergency department (ED) to standardize the care of children with bronchiolitis by implementing the use of a respiratory score to make medical decisions in patient care and limit the use of high-flow nasal cannula (HFNC) as respiratory support. However, limited literature exists regarding implementing a respiratory scoring tool within a CP and related patient outcomes or the appropriate cutoff of a respiratory score to initiate HFNC for bronchiolitis treatment.
Objective: To evaluate how using a respiratory scoring tool for decision-making, including HFNC initiation, affects patient disposition from the ED as a component of CP implementation.
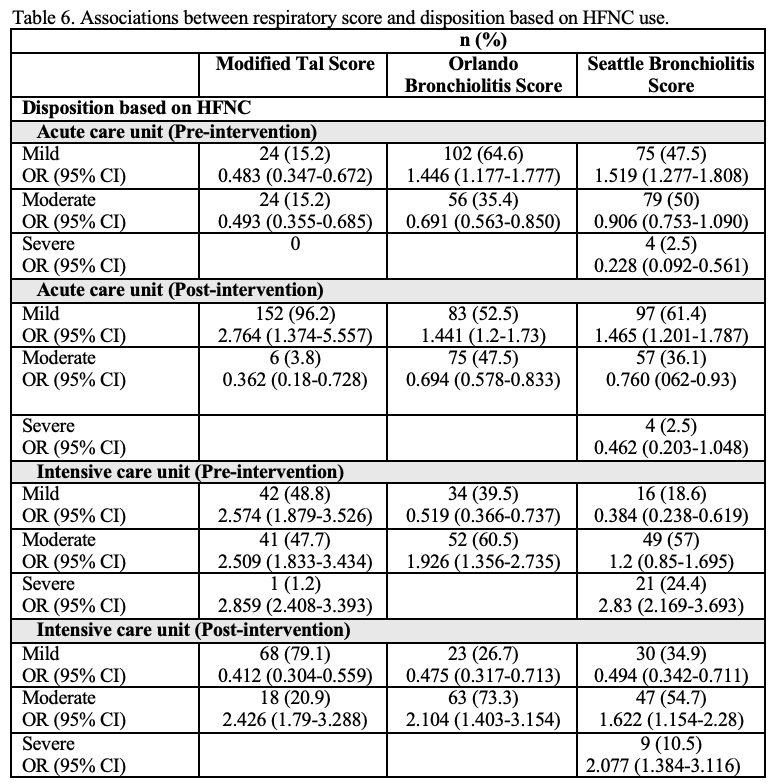
Design/Methods: We conducted a retrospective, cross-sectional study of children with bronchiolitis who visited EDs in our healthcare system. To evaluate the performance of the Seattle Bronchiolitis Score (SBS) as the respiratory score included in the CP, we calculated clinical respiratory scores using ED clinical data for three distinct respiratory scoring tools: Modified Tal Score (MTS), Orlando Bronchiolitis Score (OBS), and SBS. Each respiratory score was calculated at three time intervals: baseline, pre-HFNC, and post-HFNC. Chi-square and Kruskal-Wallis tests were performed to compare respiratory scores.
Results: We included 334 unique patients with bronchiolitis. Median age was 11 months (IQR 4-16). Children with moderate bronchiolitis were more likely to be placed on HFNC based on the OBS (OR 1.8, 95% CI 1.02-3.2) and SBS (OR 2.7, 95% CI 1.5-4.8). A HFNC intervention was significantly associated with a decrease from moderate to mild symptoms with the use of MTS (16.4%) and SBS (17.2%) but not with OBS (4.5%). Median HFNC starting settings were flow (L/kg) 1.0 (IQR 0.9-1.2) and FiO2 0.25 (0.21-0.35), respectively, irrespective of severity. Regardless of scoring tool, a score consistent with mild bronchiolitis post-HFNC was associated with acute care admission, while a moderate or severe score was associated with intensive care admission for all scores (p < 0.05). Patients with pre-HFNC scores in the moderate range were started on HFNC < 90 minutes (p < 0.05).
Conclusion(s): The choice of respiratory scoring tools for use in clinical pathways for bronchiolitis may have meaningful effects on the initiation of HFNC therapy and response to such therapy, which can affect illness trajectories and treatment decisions. Further studies are needed to determine the delta and threshold for escalation of bronchiolitis care based on respiratory scoring systems.
Parameters of each respiratory scoring system.
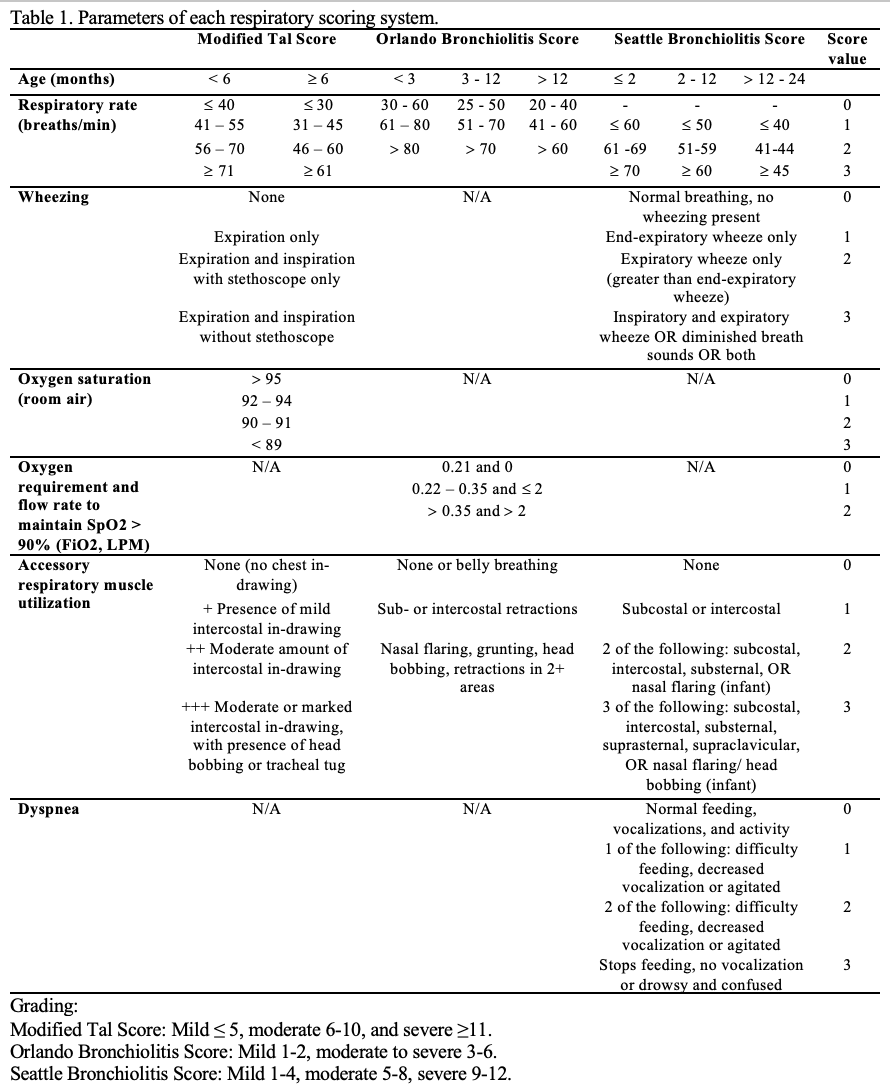
Associations between the respiratory scoring tools and initiation of high flow nasal cannula in children with bronchiolitis.
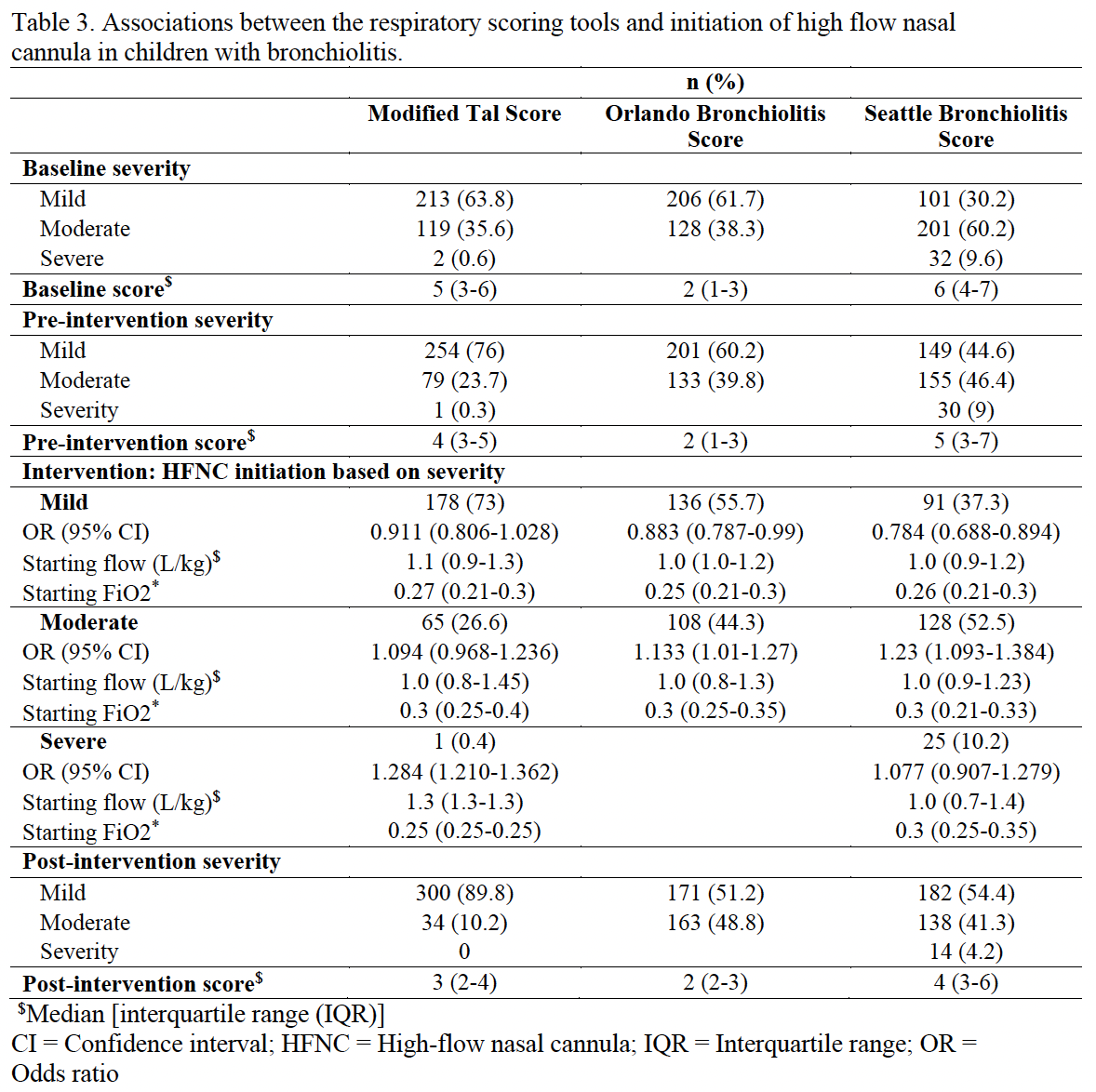
Associations between respiratory score and disposition based on HFNC use.