Endocrinology 2
Session: Endocrinology 2
307 - Applying patient-centered language and understandings to a retrospective review of pediatric patients with Variations of Sex Characteristics
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 307.3900
Tessa Meurer, University of Wisconsin School of Medicine and Public Health, Milwaukee, WI, United States; Tess Jewell, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Angelica Scribner, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Madrigal von Muchow, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Kelsey Lewis, University at Buffalo, Buffalo, NY, United States; Jennifer Rehm, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States

Tessa Meurer, MPH (they/them/theirs)
MD Student
University of Wisconsin School of Medicine and Public Health
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: Variations of sex characteristics (VSCs) is a term that refers to traits that do not align with binary expectations of “female” or “male” bodies. Intersex is another term that describes variations in sex traits; individuals may self-identify with the term intersex as a way of describing their sex or gender identity, or as a way of relating to their VSCs. Lack of clinical consensus on which diagnoses constitute VSCs has led to discrepancies in estimating the prevalence of these traits and has made creation of unified care guidelines difficult. Evolving language has further complicated both research of and care for patients with VSCs; prior terminology has been critiqued as stigmatizing or pejorative and VSCs are often framed as “disorders” for deviating from notions of a sex binary. Clear patient-centered terminology around VSCs may help ensure patients receive appropriate and affirming medical care.
Objective: We examined VSCs documented among patients at a pediatric medical center using a categorization schema based on embryological drivers of sex development rather than on binary sex.
Design/Methods: Electronic health records were screened to identify pediatric patients with VSCs seen at a large academic medical center from 2000-2023. Inclusion criteria used a broad definition of VSCs, including congenital penile variations. Diagnostic language was standardized and frequencies of VSCs were calculated and compared to national prevalence rates. Patients with VSCs were sorted into diagnostic categories: sex chromosomes, hormonal axes, internal reproductive organs, or isolated external genitalia. For patients with variations in multiple domains, cases were sorted by most upstream identified driver associated with presumed downstream effects on anatomy or physiology.
Results: A total of 1863 individuals with one or more VSC diagnoses were identified. Among these patients, 113 had variations in sex chromosomes, 52 in hormonal axes, 204 in internal reproductive organs, and 1457 in external genitalia alone. The most common anatomical VSCs were hypospadias (n=1005), chordee (n=483), and buried phallus (n=244).
Conclusion(s): The majority of identified VSCs were not associated with clear chromosomal, hormonal, or gonadal cause, but instead represented isolated external genital variations without an identified driver on the fetal sex development pathway. Reframing VSCs to decenter binary sex may improve clinical understanding of their origins and prevalence, and may also reduce patient stigma by exploring these traits not as disorders to be corrected, but as natural variations in sexual and reproductive anatomy.
MD Matriculation Confirmation with Course Completion
MD Course Completion w_ LOAs .pdf
Table 1
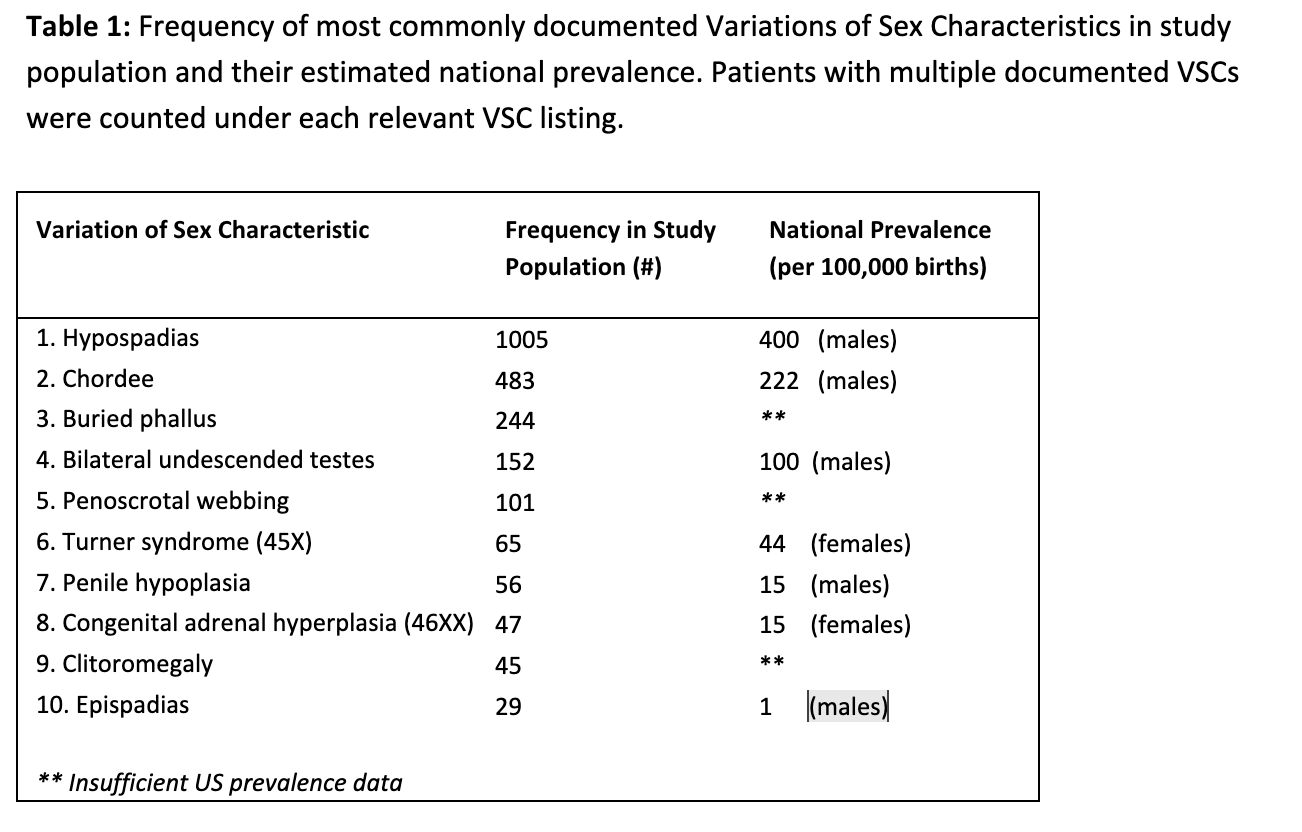 requency of most commonly documented Variations of Sex Characteristics in study population and their estimated national prevalence. Patients with multiple documented VSCs were counted under each relevant VSC listing.
requency of most commonly documented Variations of Sex Characteristics in study population and their estimated national prevalence. Patients with multiple documented VSCs were counted under each relevant VSC listing.
