Children with Chronic Conditions 2
Session: Children with Chronic Conditions 2
519 - Use of a Transition Checklist to Facilitate Youth-to-Adult Health Care Transition for Children with Medical Complexity
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 519.6759
Brittany Storhoff, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Mary L. Ehlenbach, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Kristan Sodergren, UWSMPH, Madison, WI, United States

Brittany Storhoff, DNP, FNP-BC (she/her/hers)
Nurse Practitioner
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin, United States
Presenting Author(s)
Background: Children with medical complexity (CMC) have multiple chronic conditions, high healthcare utilization, functional differences and needs beyond those of other children. Failure to adequately plan for health care transition (HCT) can lead to medical complications, discontinuity of care, increased emergency department visits and hospitalizations, and patient dissatisfaction. Support and services are lacking for HCT.
Objective: To evaluate the effectiveness and acceptability of a Transition Checklist (TC) embedded into the electronic medical record (EMR) on improving the HCT process for CMC enrolled in one pediatric complex care program, their families, and their medical providers.
Design/Methods: This mixed methods study incorporated quality improvement techniques, Lewin’s change theory and qualitative analysis to develop and refine a protocol for use of an EMR-integrated TC. The TC was developed from GotTransition resources and piloted on patients age >12 years enrolled in the complex care program. Parents’ knowledge and confidence levels about HCT were assessed before and after TC use via survey. Qualitative, written feedback from providers was analyzed using the strengths, weaknesses, opportunities, and threats (SWOT) framework.
Results: TCs were incorporated into the EMR and used to counsel patients and parents. Utilization of the TC increased from 29% to 71%. 28 surveys were collected on 14 parents before and after TC use. Knowledge of age associated steps in HCT process, confidence level in taking these steps, and overall understanding of the HCT process increased in all domains (p < 0.012, p < 0.002, p < 0.002). Five complex care providers provided written feedback. Thematic analysis revealed strengths including TC ease of use, TC facilitating accessibility of education materials during clinic visits, good receptivity of parents to TC use, and overall TC use contributing to successful facilitation of HCT. Weaknesses include need to manually upload TC into EMR, lack of automated prompts within EMR for TC use, and TC inability to overcome parents’ preference to avoid HCT discussion. Opportunities include incorporating scripting on educational topics in TC to create positive discussion on HCT and auto-uploading of TC into EMR when patient turns 12. Threats include inadequate time to use TC to discuss HCT during clinic visits.
Conclusion(s): Use of the TC facilitated improved knowledge and confidence for parents and its use was acceptable for providers. Future research includes refinement of education topics in the TC that focus on HCT outcomes.
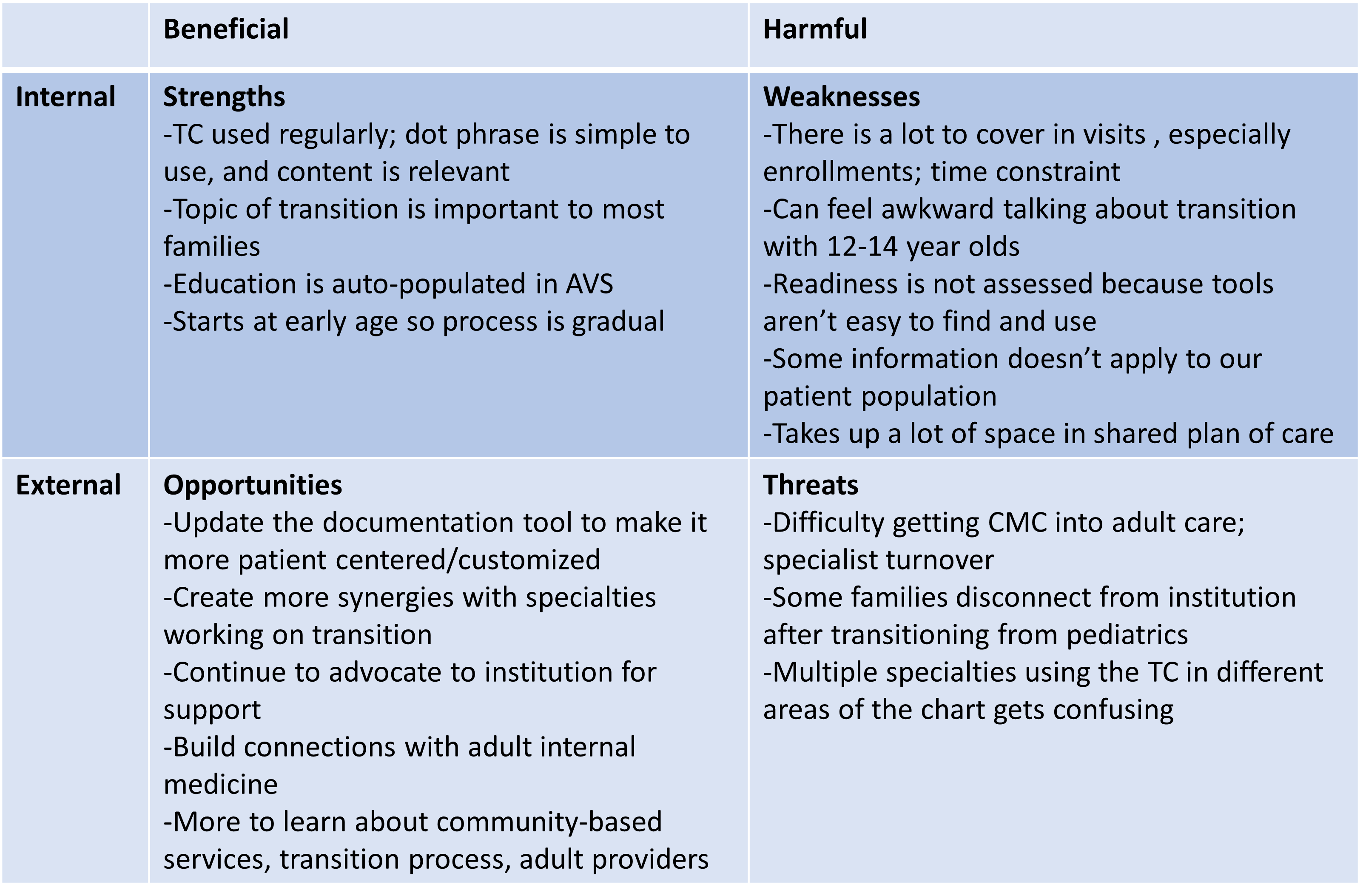
SWOT analysis – provider pre-education feedback 2019
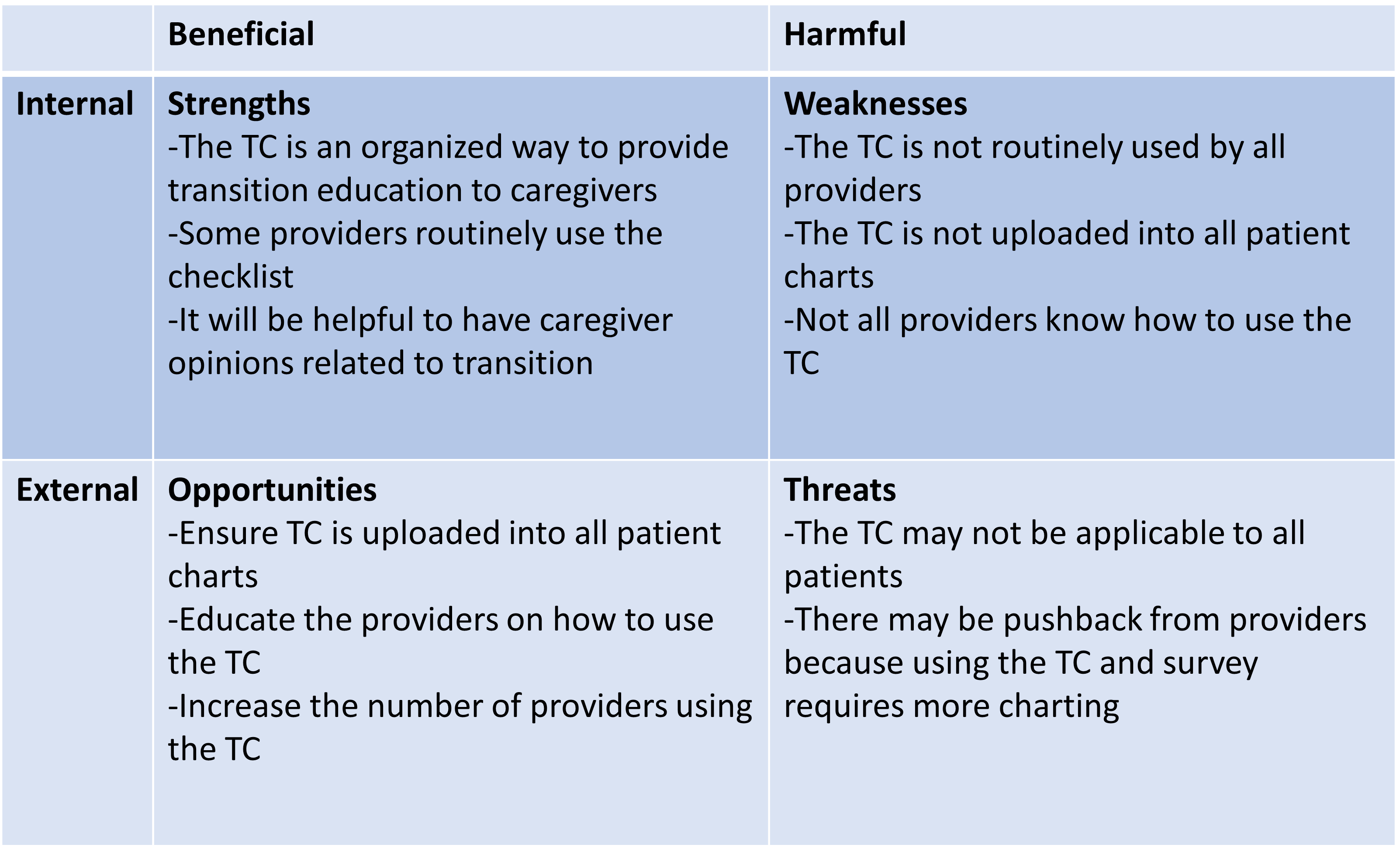
SWOT analysis – provider post-education feedback 2019
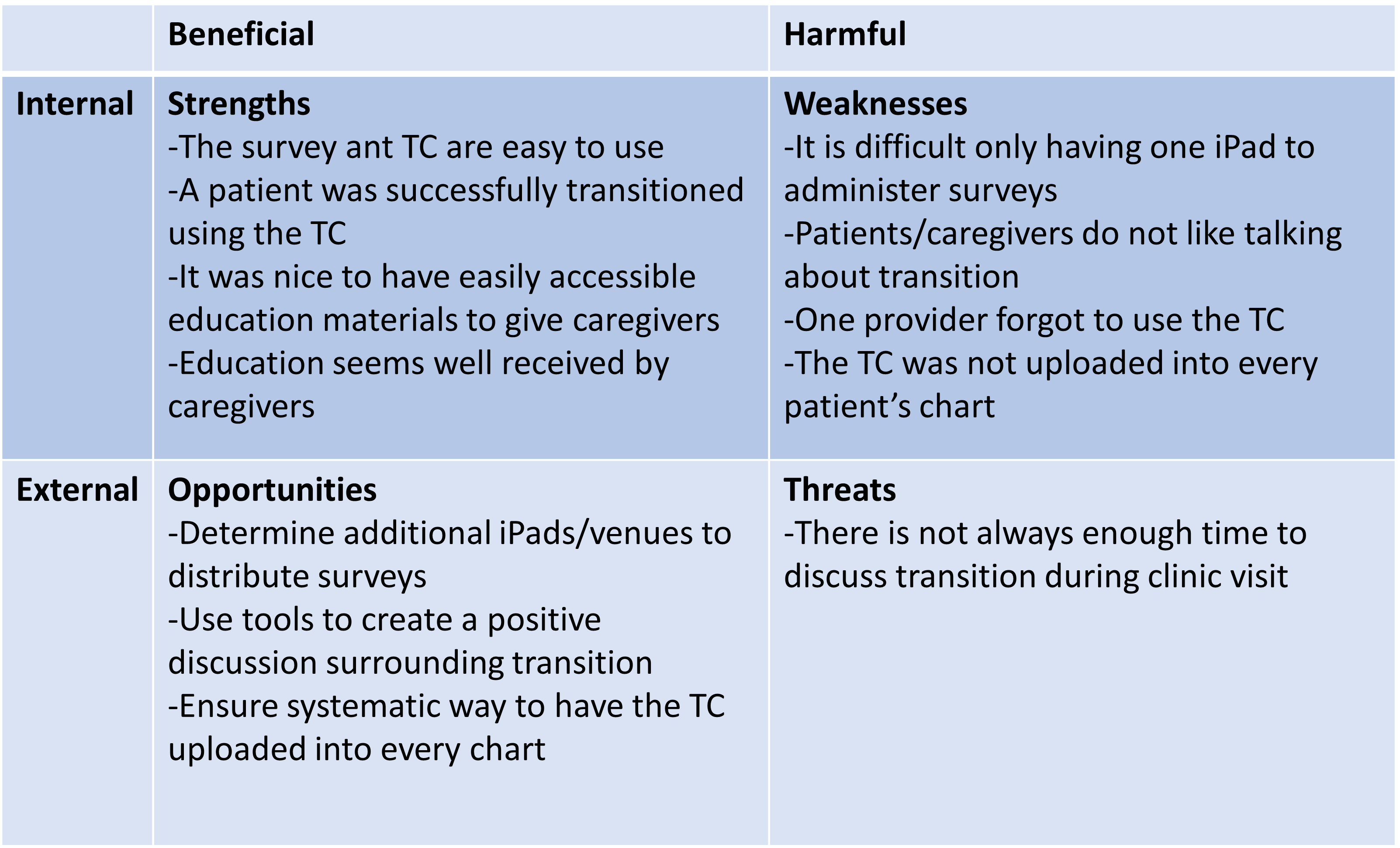
SWOT analysis – provider post-education feedback 2024