Endocrinology 2
Session: Endocrinology 2
315 - Risk Factors and Outcomes of Metabolic Bone Disease in Infants Born <27 Weeks or ≤ 750 Grams
Sunday, April 27, 2025
8:30am - 10:45am HST
Publication Number: 315.6277
Mamta Naik, Children's Memorial Hermann Hospital, houston, TX, United States; Sepideh Saroukhani, McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, TX, United States; Matthew Rysavy, McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, TX, United States; Lindsay F. Holzapfel, McGovern Medical School, University of Texas Health Science Center at Houston, Houston, TX, United States; Melissa Thoene, University of Nebraska College of Medicine, Omaha, NE, United States; Ann L. Anderson Berry, University of Nebraska College of Medicine, OMAHA, NE, United States; Amir M. Khan, McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, TX, United States; Jon E Tyson, The University of Texas Health Science Center, Houston, TX, United States; Covi Anne Tibe, McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, TX, United States; Mar Romero-Lopez, University of Texas Health Science at Houston, Houston, TX, United States

Maria del Mar Romero Lopez, MD, MS, PhD (she/her/hers)
Assistant Professor of Pediatrics. Division of Neonatology
UT Health Science Center
Houston, Texas, United States
Presenting Author(s)
Background: Metabolic bone disease (MBD) of prematurity is characterized by insufficient bone mineralization. Early diagnosis can improve outcomes, reducing fracture risk, and minimizing long-term complications.
Objective: To identify risk factors, clinical characteristics and outcomes associated with MBD in a high-risk preterm cohort.
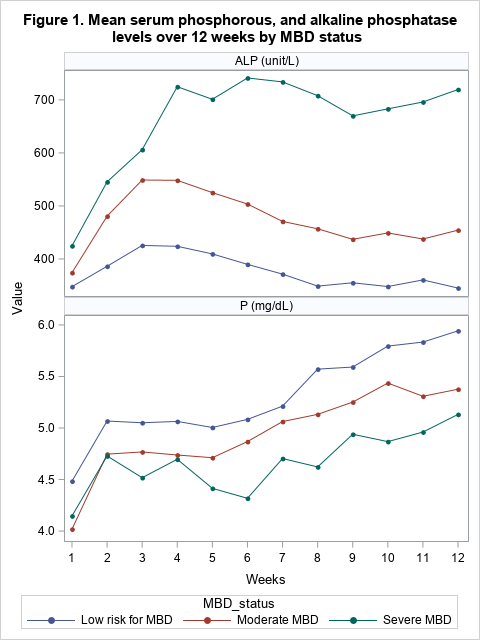
Design/Methods: A retrospective cohort study of infants born < 27 weeks or ≤750 g in a tertiary neonatal intensive care unit between 2021-2023. Infants were excluded if transferred or death occurred before 28 days. Neonates were classified as severe MBD [alkaline phosphatase (ALP) >900 unit/L and phosphorus (P) < 5.6 mg/dL], moderate MBD (ALP >700 unit/L or P < 3.1 mg/dL) and low risk for MBD without elevated markers between week 2-12 after birth. Categorical variables were compared using Chi-square or Fisher’s exact tests. Continuous data were analyzed using ANOVA or Kruskal-Wallis Test, and subsequent pairwise comparisons. Longitudinal generalized estimating equations models were used for comparison of lab data.
Results: A total of 161 infants were grouped into severe (n=28, 17.4%), moderate (n=71, 44.1%) and low MBD (n=62, 38.5%) groups (Table 1). The severe MBD group was significantly lower in gestational age (p=0.002), weight (p < 0.001), length (p=0.004), and head circumference (p=0.01). Changes in ALP levels over time significantly differed with a peak at 3-4 weeks in the moderate and severe MBD groups (p=0.008) compared with the low MBD group (Figure 1). Compared with the low MBD group, the severe MBD group had significantly later fortification of enteral feeds (23 vs 12 days), vitamin D supplementation (31 vs 16 days), and more days with parenteral nutrition in the first 28 postnatal days (24 vs 16) (all p< 0.01). The severe MBD group had significantly lower z-scores for head circumference at 36 weeks’ postmenstrual age (-2.5 vs -1.8). Compared with low MBD group, the severe MBD group had more days of assisted ventilation (48 vs 34), supplementation with oxygen at discharge (71% vs 46%), and increased incidence of retinopathy of prematurity (ROP) stage ≥2 (64% vs 37%) (all p=0.05).
Conclusion(s): Infants with severe MBD had delayed fortification, worsened growth, prolonged needs for respiratory support and greater risk of ROP. Nutritional interventions may mitigate risks for MBD. Further research is needed to prevent and treat MBD.
Baseline characteristics, nutrition, and clinical outcomes of neonates at risk for Metabolic Bone Disease (MBD)
PAS abstract Table 1.pdf
Mean serum phosphorus, and alkaline phosphatase levels over 12 weeks by MBD status