Neonatal General 6: Maternal Fetal Medicine
Session: Neonatal General 6: Maternal Fetal Medicine
156 - Extremely advanced maternal age: prevalence, outcomes and changes over recent years
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 156.5045
Aysuna Galandarova, Cleveland Clinic, Cleveland, OH, United States; Mohsen A.A.. Farghaly, Cleveland Clinic Children's, Cleveland, OH, United States; Somaya Abuelazm, Cleveland Clinic Children's, Cleveland, OH, United States; Shawana Bibi, Cleveland Clinic Children's, Cleveland, OH, United States; Hany Aly, Cleveland Children’s Hospital, Cleveland, OH, United States; Mohamed A. Mohamed, Cleveland Clinic Children's, Cleveland, OH, United States

Aysuna Galandarova Ibrahimli, MD (she/her/hers)
Research Fellow
Cleveland Clinic Children’s Hospital
Cleveland, Ohio, United States
Presenting Author(s)
Background: More women have been going through the childbearing experience later in their life. Earlier reports showed worsening pregnancy outcomes of women with advanced maternal age (AMA) compared to women aged 18-34y. However, the outcomes of women > 45y, are not well described in recent literature.
Objective: To describe recent trends in prevalence of pregnancy among women > 45 year old, their demographic disparities, clinical characteristics, and outcomes.
Design/Methods: Authors examined the National Inpatient Sample (NIS) datasets produced by the Healthcare Cost and Utilization Project (HCUP) during the years 2010-2020. Authors used the International Classification of Diseases- versions 9 (ICD9) and 10 (ICD10) codes to extract the records of women who gave birth during their hospitalization. Respective ICD9 and ICD10 codes were used to identify perinatal and clinical diagnoses, and adverse outcomes. Chi square and Fisher exact tests were used to compare frequencies and logistic regression models were used to calculate adjusted odds ratios (OR) while controlling for confounding factors.
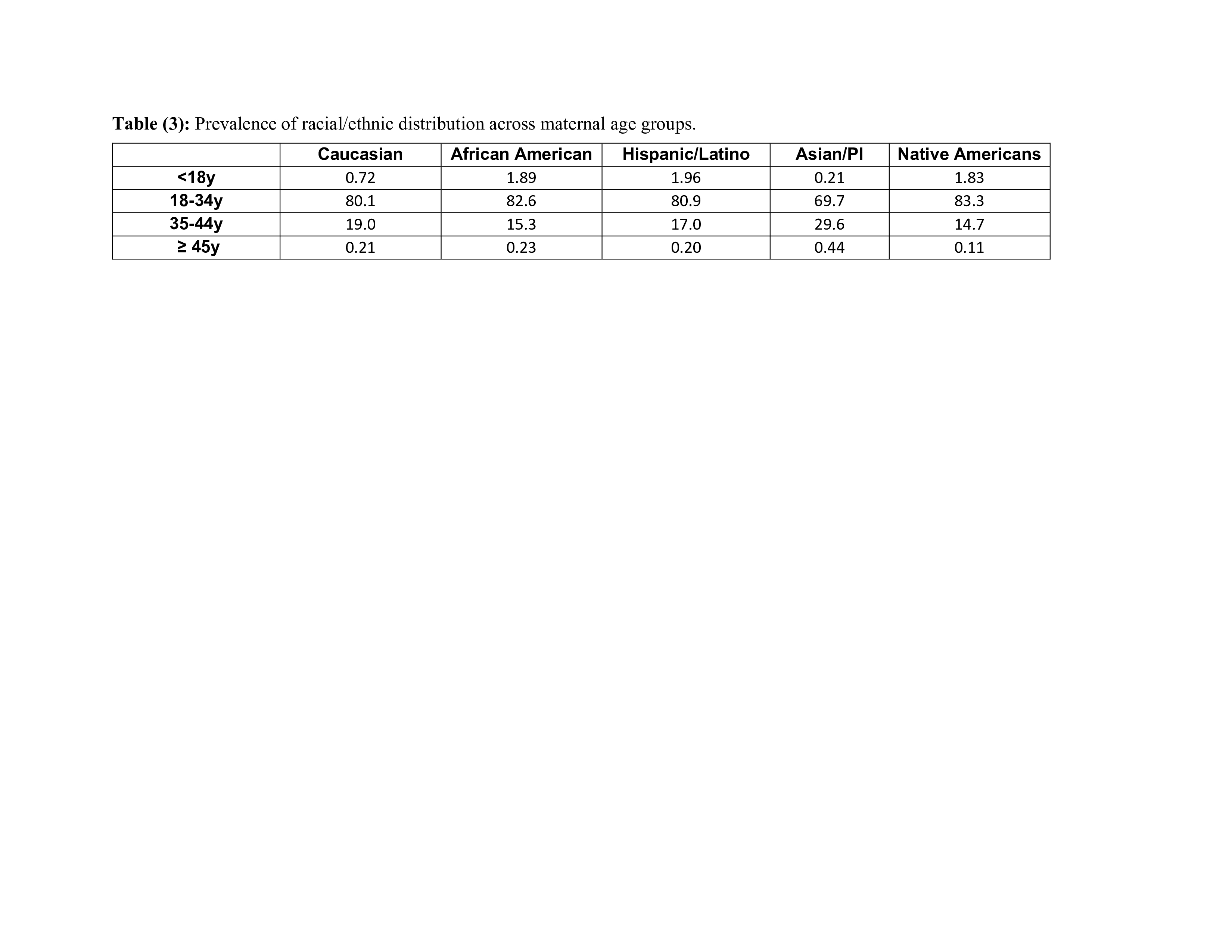
Results: The study included 42,350,892 pregnant women. Of them, 1.89% were < 18y, 81.7%% were 18-34y, 16.2% were 35-44y, and 0.21% were > 45y. The youngest to be pregnant was 9- and the oldest was 55- years old. The prevalence of pregnant women who were < 18 years old dropped from 3.17% in 2010 to 1.14%, p < 0.01. While the prevalence of pregnancy in the age of 35-44 and > 45 years increased from 14.1% to 18.9%, and from 0.20% to 0.22%, respectively, Table (1). Women > 45 years of age have significantly higher incidence to get pregnant through IVF, have multiple gestation and deliver via Cesarean deliveries, experience hypertension, gestational, or diabetes mellitus, suffer from placenta previa or placental abruption, develop perinatal hemorrhage, or sepsis, Table (2). Average, mortality among pregnant women >45 years old was 113/100,000 compared to 14, 9, & 17 in < 18y, 18-34y, or 35-44y, respectively. However, mortality in all age groups have declined over the years, p < 0.01 (Chi square test for trends). Racial/ethnic distribution varied by maternal age groups, see Table (3).
Conclusion(s): There is a slight increase in the prevalence of pregnant women > 45 years of age over recent years. They have higher chance to develop several perinatal encounters and adverse outcomes including significantly higher mortality. Healthcare providers need to be aware of these outcomes and provide proper counselling for these pregnant women.
Table (1): Change in prevalence of pregnant women by age over the years.
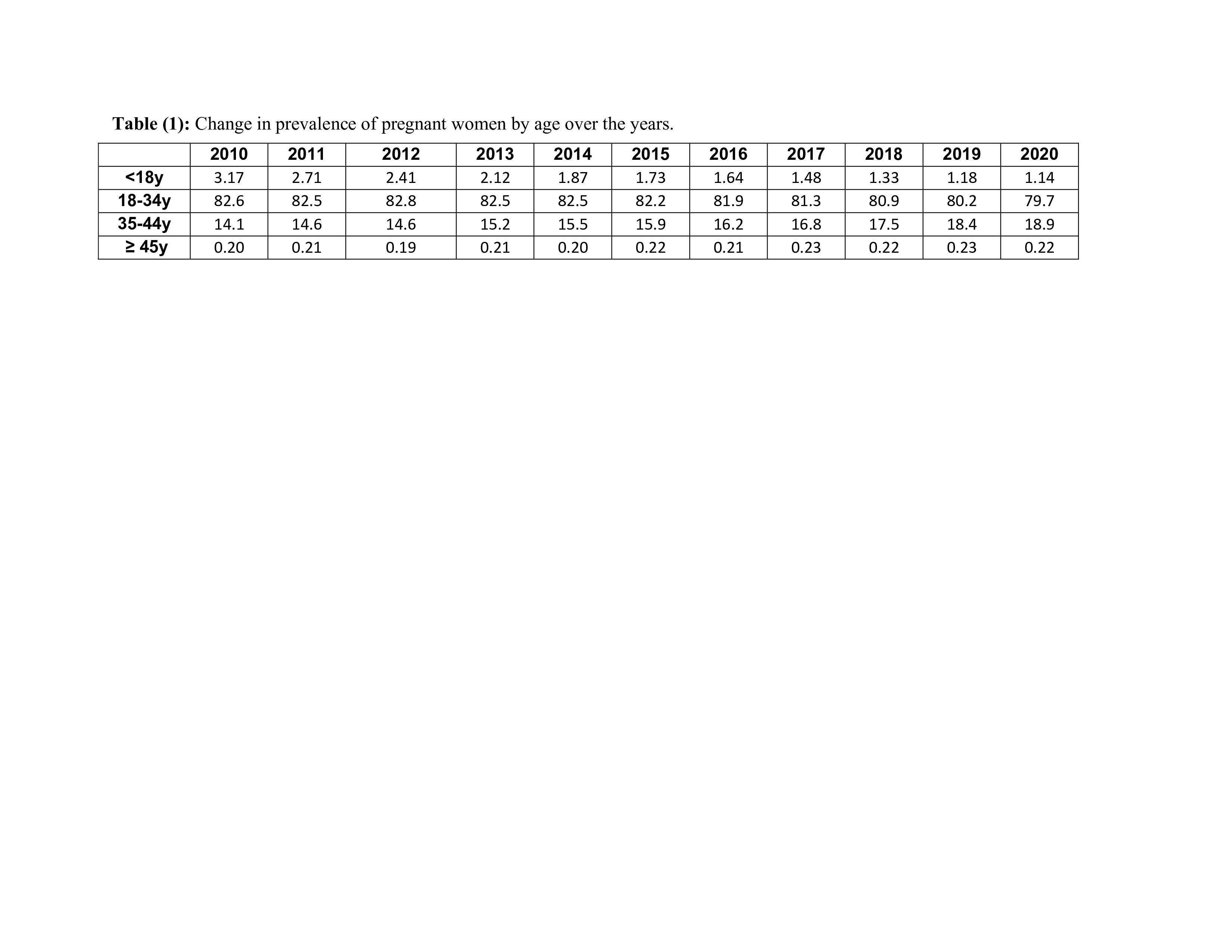
Table (2): Comparison of demographic and clinical characteristics and adverse outcomes between pregnant women ≥45 years old and pregnant women 35-44 years.
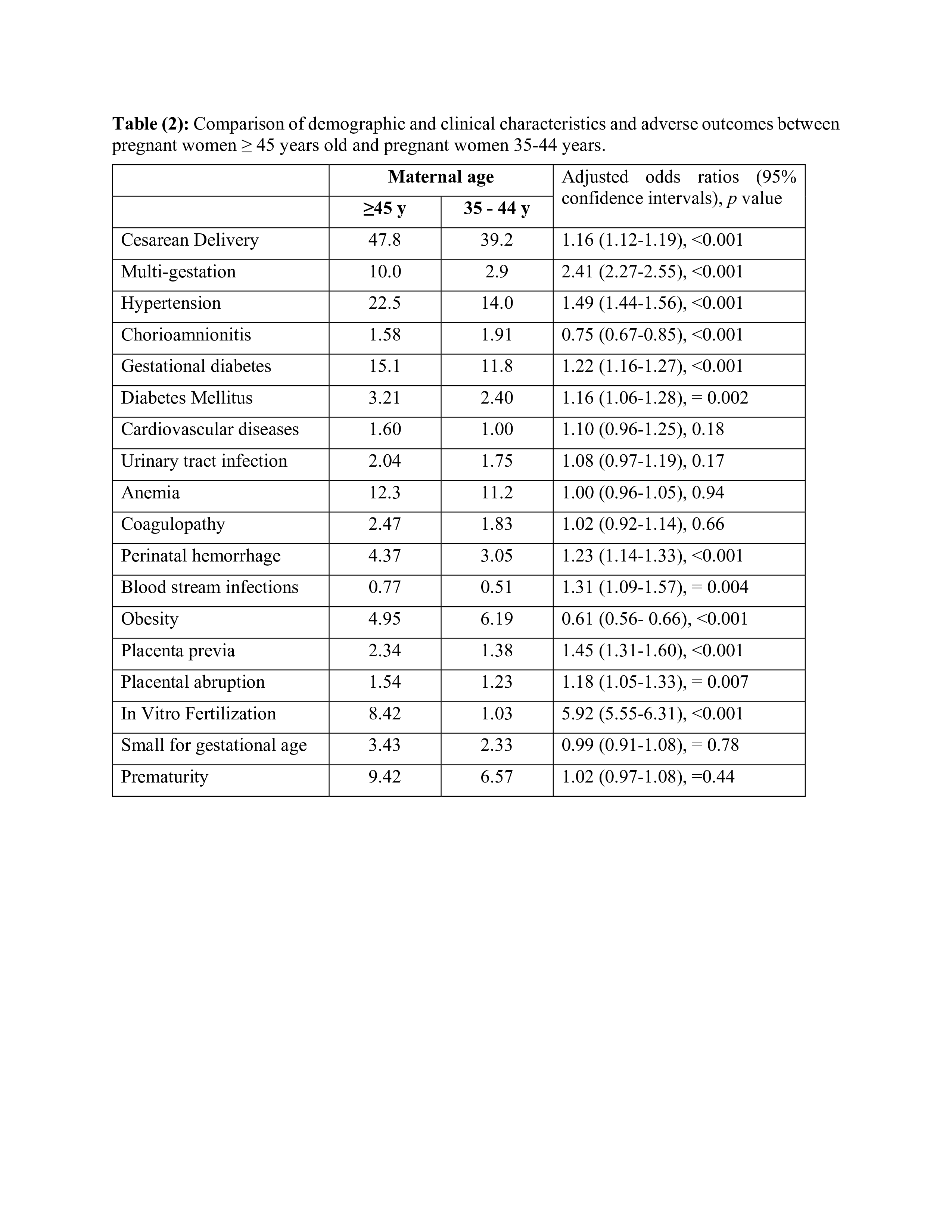
Table (3): Prevalence of racial/ethnic distribution across maternal age groups.