Quality Improvement/Patient Safety 6
Session: Quality Improvement/Patient Safety 6
493 - Strategies to Improve Golden Hour Measures in the Neonatal Intensive Care Unit
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 493.6896
Kirsten Sorum, Loyola University Chicago Stritch School of Medicine, Oak Park, IL, United States; Sachin Amin, Loyola University Chicago Stritch School of Medicine, Maywood, IL, United States; Pamela Nicoski, Loyola University Medical Center, Brookfield, IL, United States; Lindsey Young, Loyola University Chicago Stritch School of Medicine, Addison, IL, United States; Marc G. Weiss, Loyola University Chicago Stritch School of Medicine, Maywood, IL, United States
- KS
Kirsten Sorum, DO (she/her/hers)
Neonatology Fellow
Loyola University Chicago Stritch School of Medicine
Oak Park, Illinois, United States
Presenting Author(s)
Background: Interventions both at the time of delivery and in the immediate time period following delivery are critically important to the outcomes of neonates. These include practices such as delayed cord clamping, thermoregulation, and prompt treatment of hypoglycemia, respiratory distress syndrome and sepsis.
Objective: To continually improve and sustain Golden Hour measures within our Neonatal Intensive Care Unit (NICU).
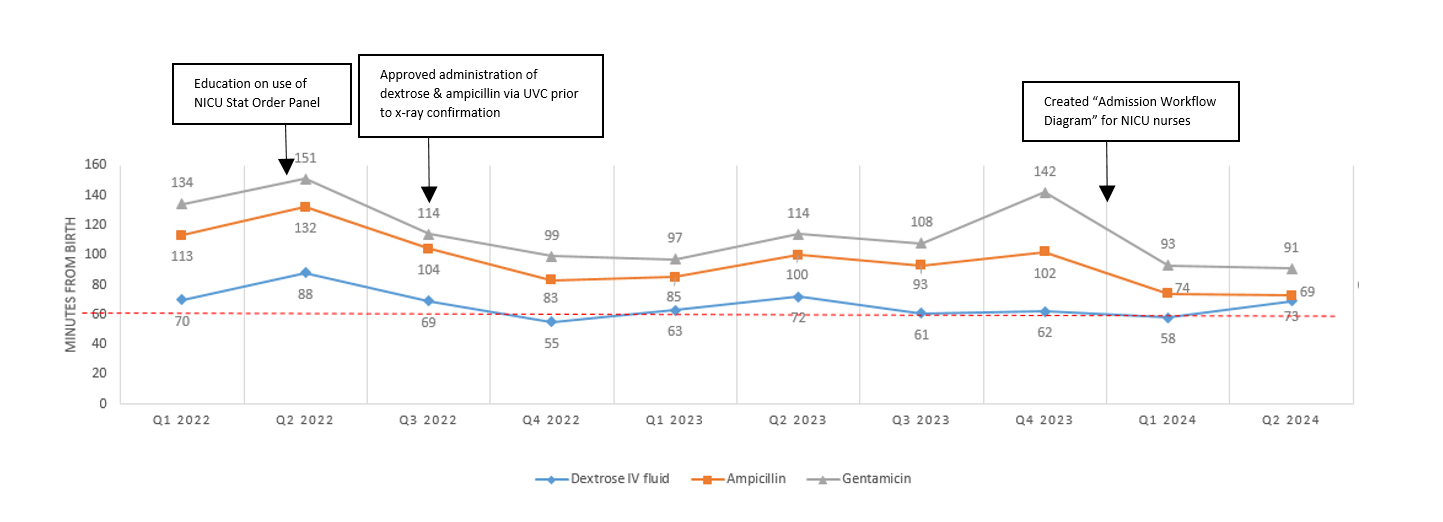
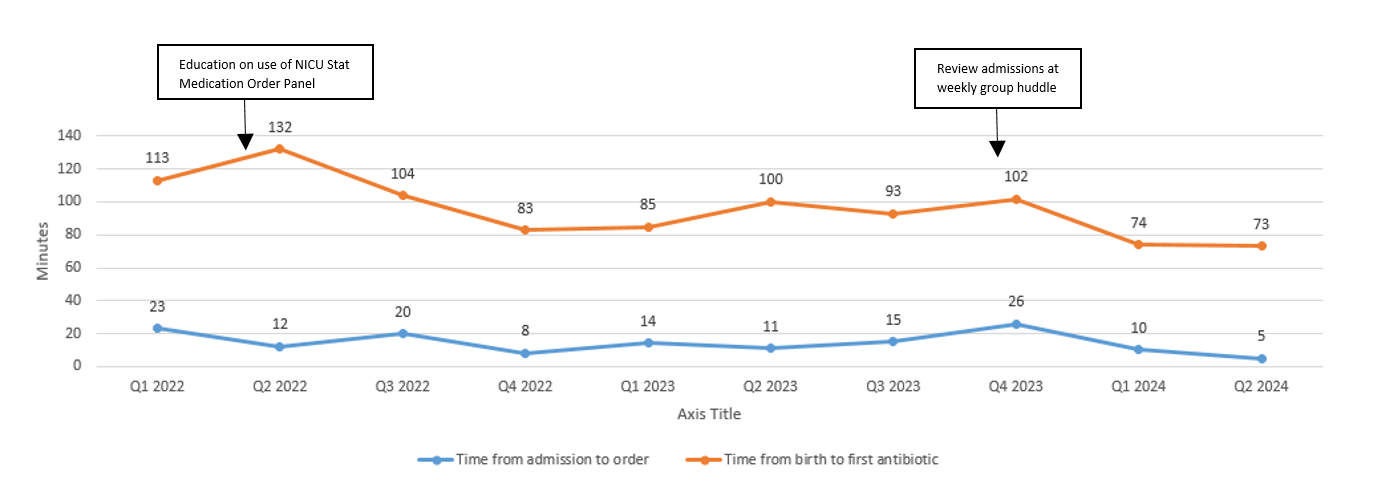
Design/Methods: A Golden Hour team was organized consisting of physician champions, nurses, and pharmacists. Different goals and subset teams were created focusing on specific measures within Golden Hour. These included improvement in admission neonatal temperatures, time to intravenous (IV) dextrose and antibiotics, as well as time to surfactant. The data within each goal continues to be monitored and areas of focus and improvement are identified. Some examples of specific interventions to improve the Golden Hour goals include: weighing the neonate in the delivery room, pre-admitting patients into the electronic medical record, prompt communication between the delivery and NICU team, the use of long umbilical cords for initial bloodwork, the implementation of a “Stat NICU Medication” order set, inserting a peripheral IV catheter prior to umbilical venous catheter (UVC) placement, allowing infusion of IV fluids and ampicillin through UVC prior to radiologic confirmation, and a protocol for surfactant administration within the first ninety minutes of life.
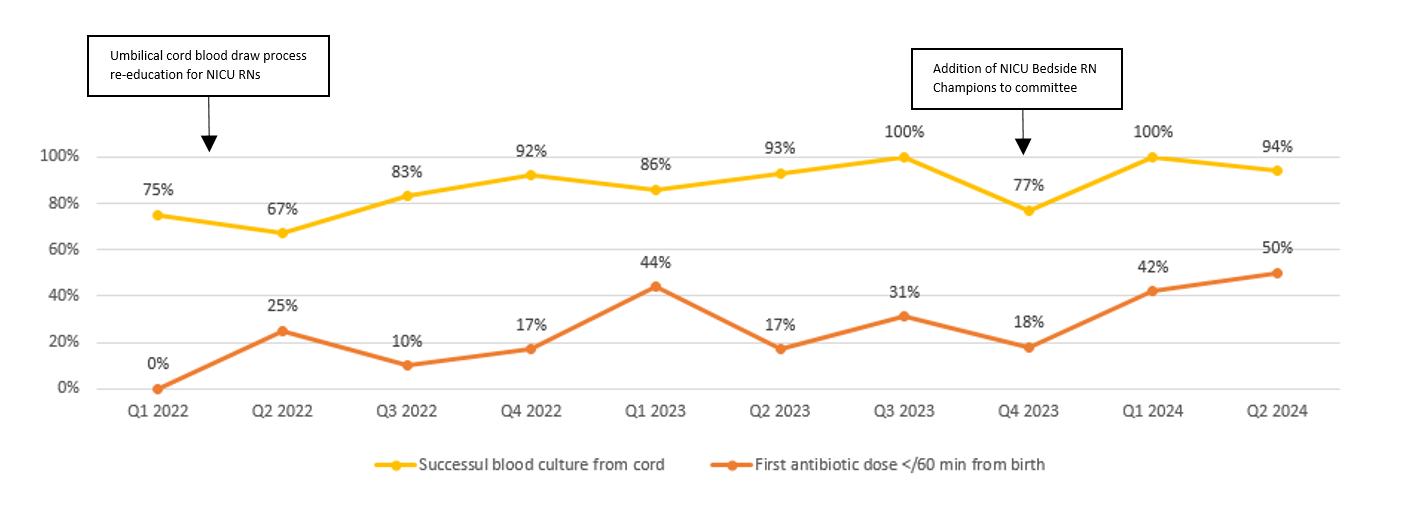
Results: Since 2022, our team has been able to continually improve and expand upon various Golden Hour initiatives by instituting a dedicated team that regularly assesses data and intervenes with Plan-Do-Study-Act (PDSA) cycles. Our multifaceted approach has allowed our unit to continuously improve various Golden Hour measures. The average time to order antibiotics from admission has decreased from 23 minutes to 5 minutes. The average time to first antibiotic dose from birth has improved from 113 minutes to 73 minutes, and our percent of patients receiving their first antibiotic dose within one hour life has improved from 0% to 50%. Our average time to dextrose administration has also continued to downtrend over the past two years. New areas of focus include decreasing time to surfactant administration and maintaining appropriate admission temperatures.
Conclusion(s): The formation of a Golden Hour team as well as subset teams allowed us to improve various measures within Golden Hour. Continuous data tracking and subsequent interventions to improve Golden Hour achievement have allowed us to sustain, troubleshoot, as well as improve our initiative.
Average Time to Administration of Dextrose and Antibiotics
Time to Antibiotic Orders (from Admission) and Time to First Antibiotic (from Birth)
Successful Long Umbilical Cord Blood Culture and Achievement of First Antibiotic Dose within Golden Hour