Neonatal Quality Improvement 5
Session: Neonatal Quality Improvement 5
524 - Supporting Tiny Lungs: A Quality Improvement Initiative to Reduce Delivery Room Intubation in Preterm Infants
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 524.6543
Melody Chiu, University of Texas Southwestern Medical Center, Dallas, TX, United States; Heather Weydig, Nationwide Childrens, Columbus, OH, United States; Britni B. Maple, University of South Carolina School of Medicine, Prisma Health, Greenville, SC, United States; Amelia Snead, Parkland, Dallas, TX, United States; Valerie Simcik, Parkland, Dallas, TX, United States; Asmahan Ahmed, University of Texas Southwestern, Dallas, TX, United States; L. Steven Brown, Parkland Health, Dallas, TX, United States; VENKATAKRISHNA KAKKILAYA, UT Southwestern Medical Center, Dallas, TX, United States

Melody Chiu, MD (she/her/hers)
Assistant Professor
University of Texas Southwestern Medical Center
Dallas, Texas, United States
Presenting Author(s)
Background: Avoiding delivery room intubation (DRI) is associated with decreased incidence of bronchopulmonary dysplasia (BPD) and/or death. The implementation of a resuscitation bundle has previously decreased DRI rates at our institution. However, the noted improvement was largely limited to infants born at 26-29 weeks’ gestational age (GA). There is limited data on strategies to decrease intubation rates in ≤ 25 weeks GA infants.
Objective: To decrease DRI among infants born ≤ 25 weeks from 55% to 45% within 36 months through longitudinal quality improvement efforts.
Design/Methods: A single center QI project included preterm infants born at 22-25 weeks’ GA who were endotracheally intubated in the delivery room and required invasive mechanical ventilation. An updated resuscitation bundle was implemented, including longer duration of PPV in absence of bradycardia, increase in peak inspiratory pressure and/or positive end expiratory pressure, avoidance of hypoxia, pre-and post- intubation huddle, and debriefing. The Plan-Do-Study-Act (PDSA) cycle framework guided the iterative process. Pre-QI cohort (January 2019-June 2021) were compared with post-QI cohort (July 2021-June 2024).
Results: Of the 214 infants born in the study period, 89 infants belonged in the pre-QI cohort (Pre-QIC) and 125 belonged to the post-QI cohort (Post-QIC). After excluding infants who received comfort care in the delivery room, 81 infants were born in Pre-QIC and 115 infants were born in Post-QIC. A special cause variation was noted with decrease in intubation rate in the second half of 2021. DRI rates decreased from 56% to 43% from Pre-QIC to Post-QIC. Infants in Post-QIC were lower in GA (23 vs. 24 weeks, p = 0.03) compared to Pre-QIC with no difference in birth weight (620g vs 650g, p = 0.44). Compliance with standardized ventilation corrective steps improved from 88% to 98%, and higher maximum positive end expiratory pressure (PEEP) was used in Post-QIC (6 vs 5 cm H2O, p = 0.02). Infants in Post-QIC had lower rates of pneumothorax (2% vs 19%, p < 0.01), and pulmonary interstitial emphysema (12% vs. 33%, p = 0.02). Rates of BPD, severe intraventricular hemorrhage, severe retinopathy of prematurity, and mortality were similar.
Conclusion(s): Our study demonstrates that DRI rate can be decreased in 22-25 weeks’ GA infants with a QI bundle focused on improving non-invasive face mask ventilation. Decreased intubation rates decreased the incidence of pneumothorax in infants intubated in the delivery room. Our study findings should be confirmed in larger multicenter studies.
Figure 1. Study Flow of Participants
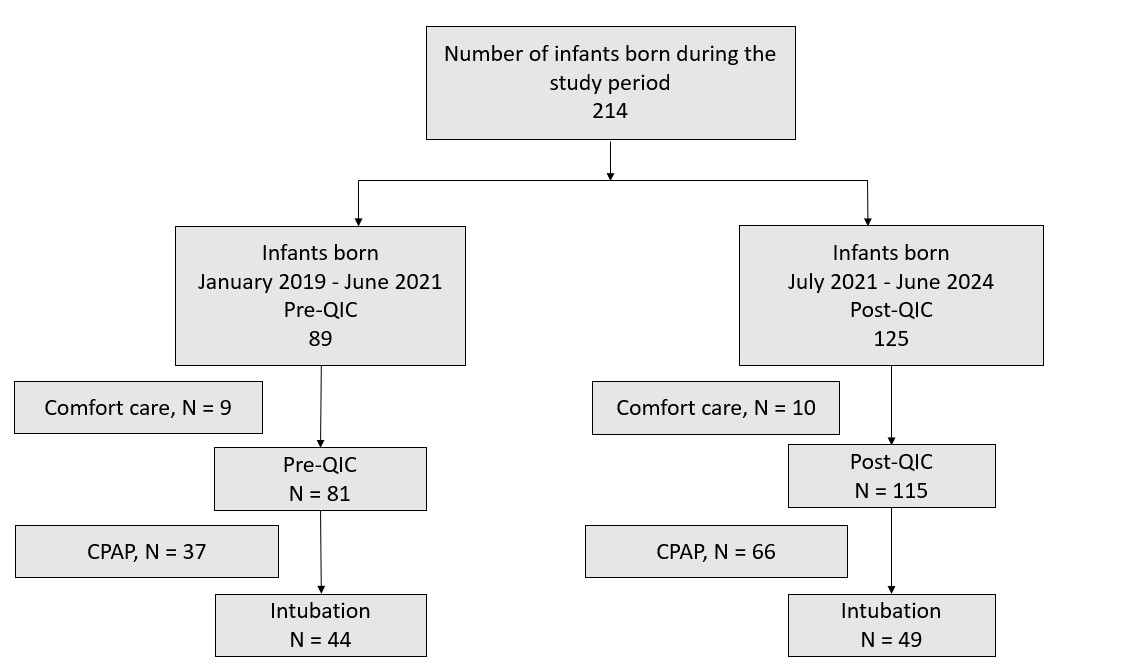
Figure 2. Control Chart for Delivery Room Intubation Rates
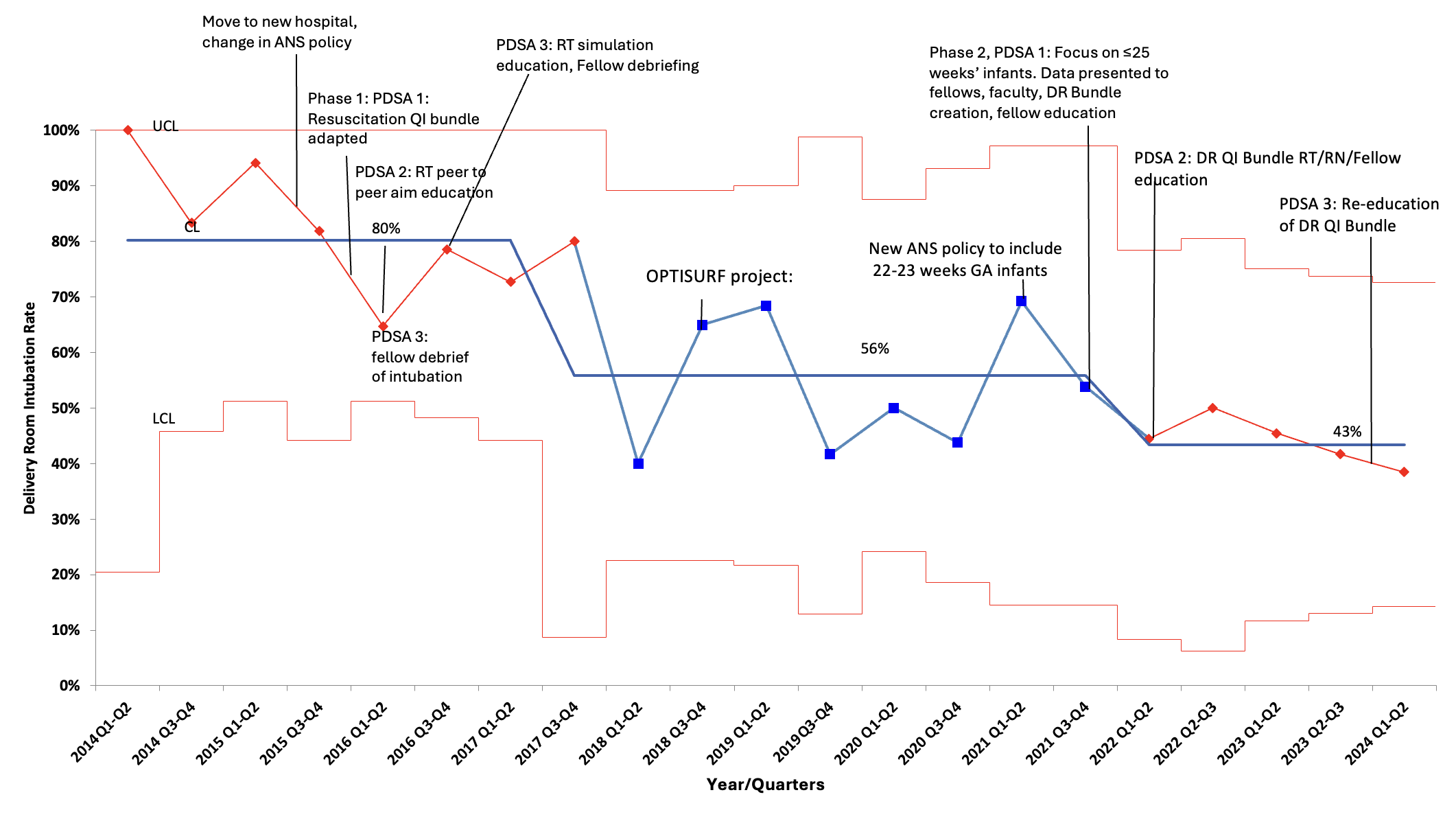
Table 1. Maternal and Neonatal Factors, Neonatal Clinical Outcomes
.jpg)
Figure 1. Study Flow of Participants
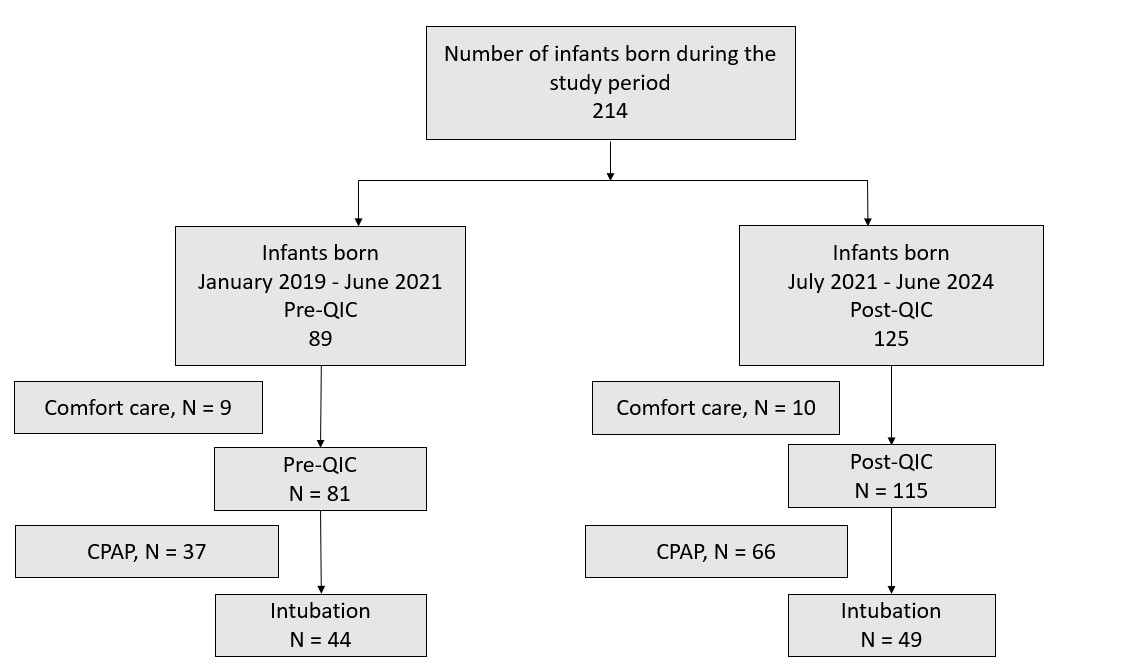
Figure 2. Control Chart for Delivery Room Intubation Rates
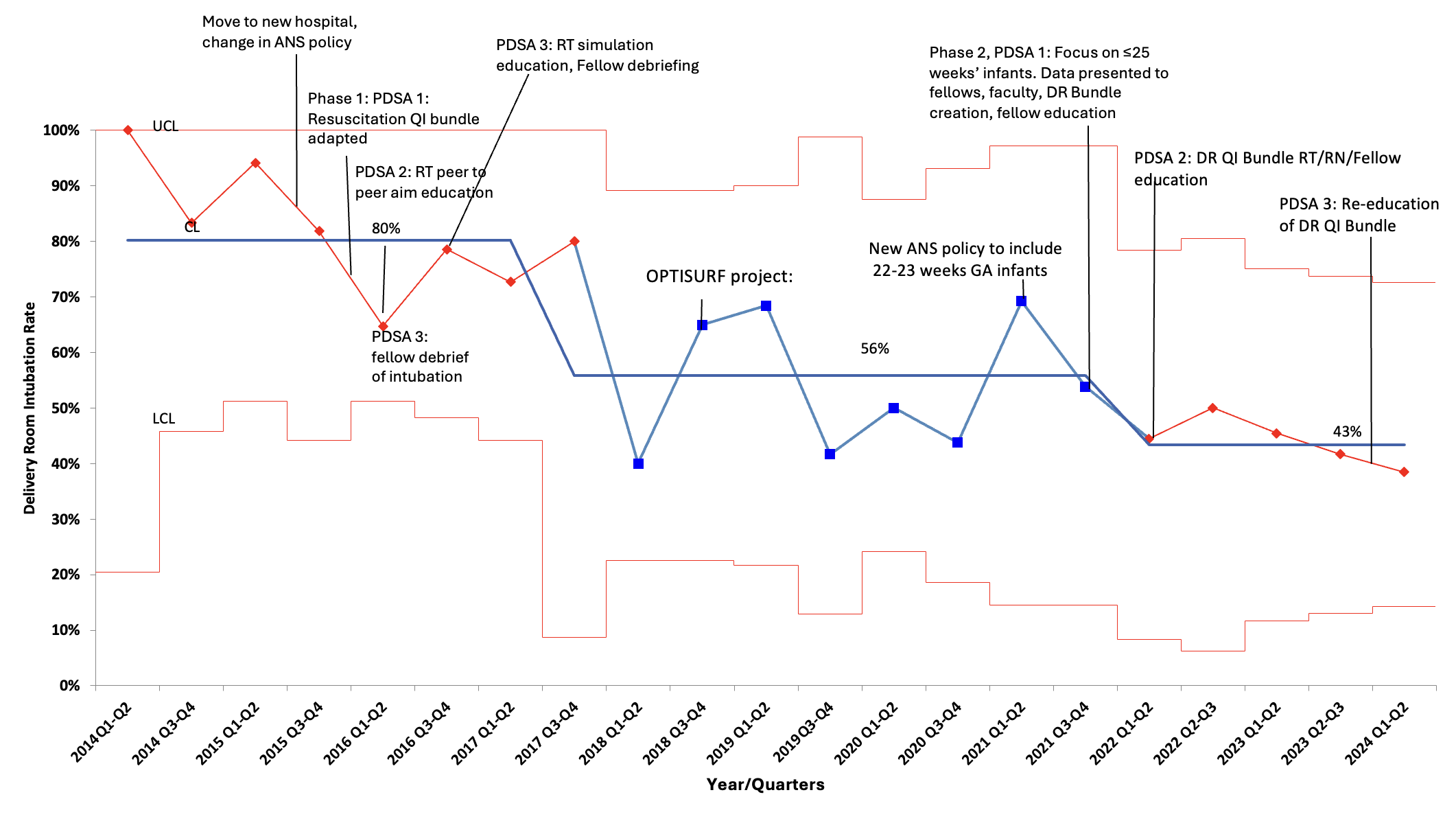
Table 1. Maternal and Neonatal Factors, Neonatal Clinical Outcomes
.jpg)


