Neonatal Quality Improvement 6
Session: Neonatal Quality Improvement 6
540 - Postpartum Depression Screening in the NICU: A Quality Improvement Initiative
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 540.6334
Chelsey A. Bithell, Georgetown University School of Medicine, Chevy Chase, MD, United States; Karen L. Kamholz, MedStar Georgetown University Hospital, Arlington, VA, United States; Shilpa Saroop, Georgetown University School of Medicine, Silver Spring, MD, United States

Chelsey A. Bithell, MD (she/her/hers)
Fellow
MedStar Georgetown University Hospital
Chevy Chase, Maryland, United States
Presenting Author(s)
Background: Postpartum depression (PPD) is a mood disorder that arises in parents during or after pregnancy. Rates of PPD are increasing, and parents in the NICU are at increased risk with negative associated parent and child outcomes. Given this, our NICU developed a guideline to screen both NICU parents at two weeks, one month, and monthly until discharge.
Objective: Improve compliance with PPD screening in a Level IV academic NICU and connect parents with positive PPD screens with psychology and social work resources. This project aims to improve screening rates of both parents in our NICU to over 80% in 1 year.
Design/Methods: We utilized the Model for Improvement. Our multidisciplinary team included a resident, NICU fellow, attending physician, nurses, NICU patient navigator and NICU psychologist. Our outcome measure was the percentage of screens completed. Process measures were percentage of providers who knew the process for screening and number of parents receiving screens at appropriate times. A balancing measure was increased charting time for nurses to enter results into the EMR and to email appropriate individuals about positive screens. Interventions included educating doctors and nurses about PPD, surveying providers about barriers to screening, including screening in daily progress notes, discussing screening during rounds, placing screens and resources at bedside for parents, sending weekly emails to QI team indicating parents due for screening, and placing this list in the doctor work area at the beginning of every week.
Results: Prior to the initiation of this project, our PPD screening completion rate was 25%. Following our interventions, our screening rates increased to 56% (Fig 1). Overall, we were more successful in screening mothers compared to fathers (Fig 2). While both residents and nurses agreed that the greatest barrier was having higher-acuity tasks to focus on as well as a tendency to forget the screening requirement, nurses additionally reported discomfort in discussing mental health with parents (Fig 3).
Conclusion(s): Our efforts have led to a modest improvement in PPD screening of our NICU parents. We are encouraged by the increasing trend in screening, but compliance is still quite variable. An important area for improvement is increasing screening of our fathers. Future directions include starting "Mental Health Monday's" to aid with consistency, creating an automatic alert to notify the unit psychologist of positive screens, and sending a survey to NICUs across the county to learn what other units are doing for parents’ mental health.
Figure 1: Parents Screened Over Time
.jpg) PPD screening completion rate between November 19th and October 6th. Interventions noted in red boxes. Total percentage of screens completed has improved from about 25% at the start of the study to 56% over a period of one year.
PPD screening completion rate between November 19th and October 6th. Interventions noted in red boxes. Total percentage of screens completed has improved from about 25% at the start of the study to 56% over a period of one year.Figure 2: Screening breakdown of mothers vs fathers
.jpg) PPD screening completion rate for mothers and fathers. Compliance for fathers is generally lower than for mothers.
PPD screening completion rate for mothers and fathers. Compliance for fathers is generally lower than for mothers.Figure 3: Pareto Chart: Perceived Barriers to Screening
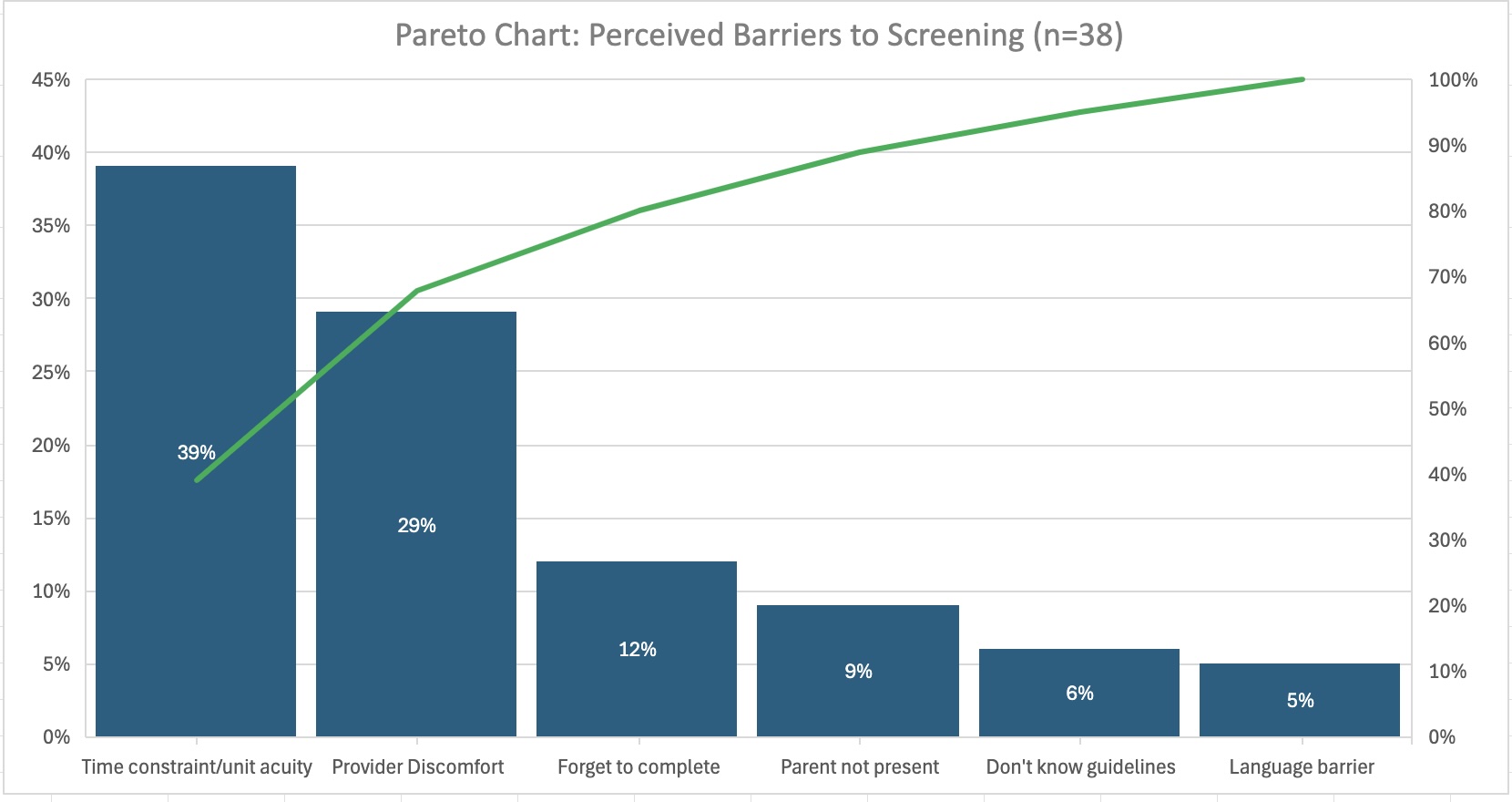 Pareto chart illustrating the barriers to completing PPD screening as reported by nurses and residents. Key concerns include prioritizing higher acuity tasks in the NICU, discomfort discussing mental health, and the tendency to forget the screening requirement.
Pareto chart illustrating the barriers to completing PPD screening as reported by nurses and residents. Key concerns include prioritizing higher acuity tasks in the NICU, discomfort discussing mental health, and the tendency to forget the screening requirement.

