Critical Care 4
Session: Critical Care 4
504 - Paracorporeal Ventricular Assist Device Implant and Rehabilitation in Children
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 504.5981
Amaryllis Fernandes, Texas Children's Hospital, HOUSTON, TX, United States; Chetna Pande, Baylor College of Medicine, Waco, TX, United States; Robin Schlosser, Baylor College of Medicine, Houston, TX, United States; Melissa Lusby, Baylor College of Medicine, Houston, TX, United States; Hari Tunuguntla, Baylor College of Medicine, Houston, TX, United States; Barbara Ann. Elias, Texas Children's Hospital, Houston, TX, United States; Dawn Wilson, Baylor College of Medicine, Houston, TX, United States; Iki Adachi, Baylor College of Medicine, Houston, TX, United States; Joseph Spinner, Baylor College of Medicine, Houston, TX, United States; Kriti Puri, Baylor College of Medicine, Houston, TX, United States

Amaryllis Fernandes, MD
Resident
Texas Children's Hospital
HOUSTON, Texas, United States
Presenting Author(s)
Background: here is very limited data regarding pediatric rehabilitation after paracorporeal (pc) ventricular assist device (VAD) implant and its impact on post-heart transplant (HTx) outcomes.
Objective: Our study sought to explore the connection between rehabilitation and early mobilization in patients with pcVADs and post-HTx outcomes.
Design/Methods: This single center retrospective cohort study includes all patients (pts) < 18 years old undergoing pcVAD implant from 01/2017 to 12/2022. Physical (PT) and occupational therapy (OT) and nutritional rehabilitation were tracked after VAD implant through post-HTx discharge/death. To account for neurodevelopmental differences, results are reported in 3 groups based on age at implant – infant/young toddler ( < 2 years), toddler (2-5 years), and child (≥6 years)
Results: Forty pts were included: 31 infants (median age 4.1mo), 6 toddlers (median age 3.6yr), and 3 children (median age 7.5yr). Underlying diagnosis included 21 (53%) cardiomyopathy (CM), 17 (43%) single ventricle congenital heart disease (svCHD) and 2 (5%) biventricular (biv) CHD. At VAD implant, 9 pts (23%) were INTERMACS 1, 29 (73%) were INTERMACS 2, and 2 (4%) were INTERMACS 3.
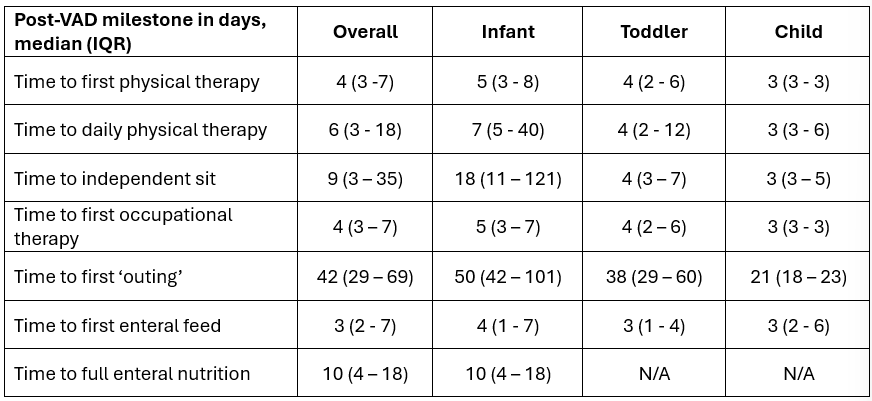
Table 1 shows rehabilitation metrics post-VAD implant. The median number of PT sessions increased from 2 (IQR 1 - 4) in the 1st wk post-VAD to 4 (IQR 2-7) in the 2nd wk post-VAD. After pcVAD implant, 31 pts (77.5%) progressed to doing daily PT prior to HTx; INTERMACS stage ≥2 at VAD implant was associated with greater likelihood of achieving this goal (84% vs 44% in INTERMACS 1, p=0.029).
Twenty-five pts (63%, all infants) advanced to fully enteral nutrition. Pts with CM (86%) were more likely to meet this milestone than those with sv- or biv-CHD (35%, 50%, p = 0.006).
Thirty-two pts (80%) survived to HTx (8 infants died on VAD). By the time of transplant, 26 patients (65%) were able to meet or exceed their pre-VAD physical activity baseline. Post-HTx length of stay had a positive correlation with time to 1st feed post-VAD (r = 0.374, p = 0.042) and time to 1st PT post-VAD (r = 0.394, p = 0.031). Additionally, post-HTx length of stay was significantly impacted by whether or not patients were able to regain their pre-VAD physical activity baseline (p=0.021).
Conclusion(s): We describe granular rehabilitation metrics that are vital for benchmarking and quality improvement efforts for early mobilization after pediatric VAD implantation Early mobilization on pcVAD support is associated with shorter post-HTx hospitalization.
Post-VAD Rehabilitation Milestones