Adolescent Medicine 3: E-Cigarettes & Other Substances
Session: Adolescent Medicine 3: E-Cigarettes & Other Substances
111 - Mental Health Comorbidities among Youth Presenting for a Substance-Related Visit to a Children’s Hospital, 2016-2021
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 111.6022
Alexis Ball, Seattle Children's, North Bend, WA, United States; Anthony L. Bui, University of Washington/Seattle Children's, Seattle, WA, United States; Kym Ahrens, Seattle Children's Research Institute, Seattle, WA, United States
- AB
Alexis Ball, MD MPP
Acting Assistant Professor
Seattle Children's
North Bend, Washington, United States
Presenting Author(s)
Background: Adolescence is a critical window in which substance use and mental health conditions emerge. There has been increasing healthcare utilization for these conditions, yet there is limited data describing the burden of mental health comorbidity among substance-related healthcare visits.
Objective: To assess: 1) mental health comorbidity among substance-related visits and 2) identify trends and odds of presenting with any mental health comorbidity by substance type.
Design/Methods: We conducted a cross-sectional study of the Pediatric Health Information System (PHIS) database of substance-related visits (SRV) from January 2016 through December 2021 among youth aged 12-21 years. SRVs were defined by ICD-10-CM codes for substance ‘use’, dependence, or overdose for alcohol, cannabis, nicotine, opioids, sedatives, stimulants, hallucinogens, or other substances. Visits were characterized by demographic characteristics, substance type(s), and associated mental health diagnosis. Loess regression was utilized to observe trends over time. Generalized linear mixed models were used to estimate odds ratios of presence of mental health comorbidity by encounter and substance type, adjusting for age, race/ethnicity, and sex.
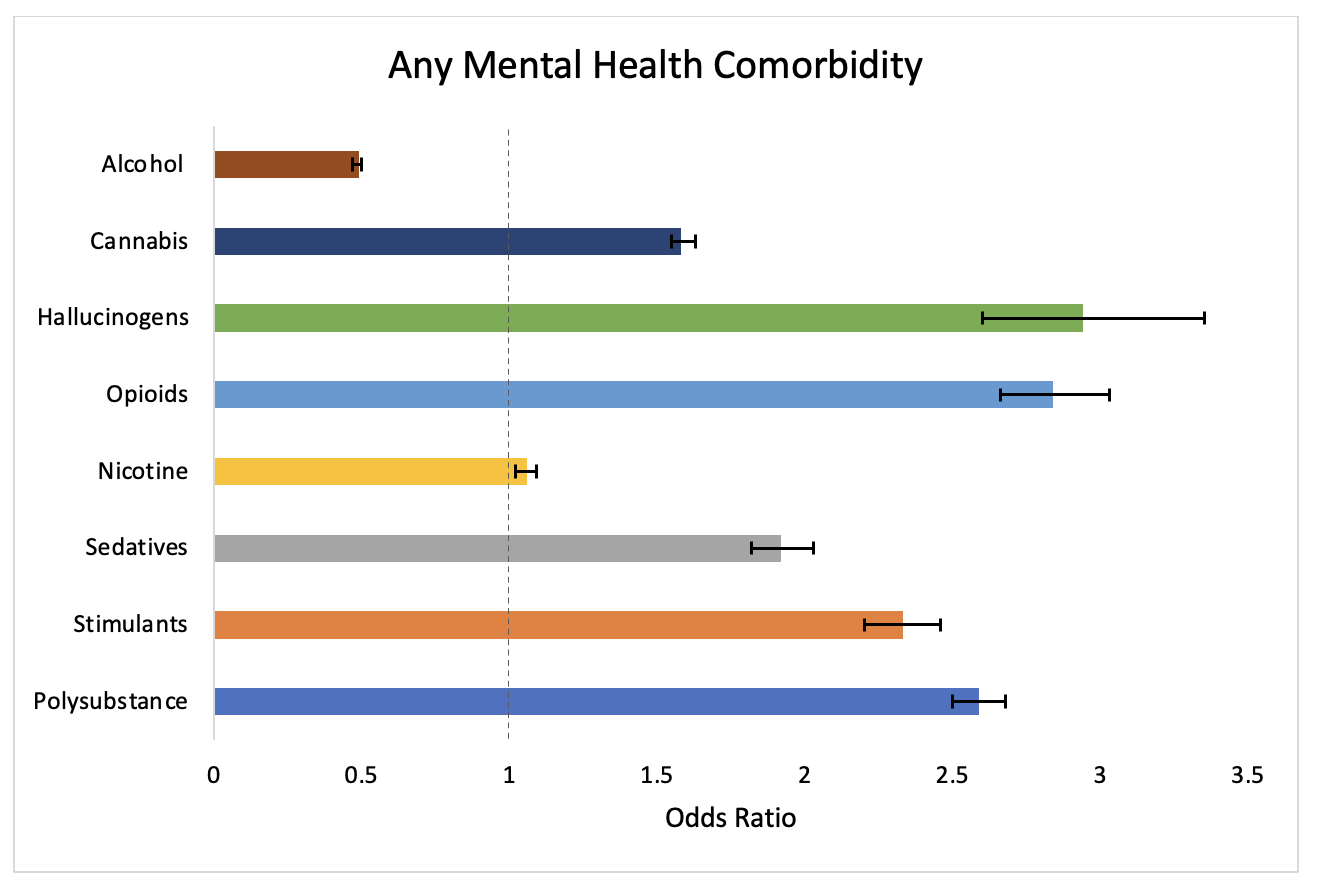
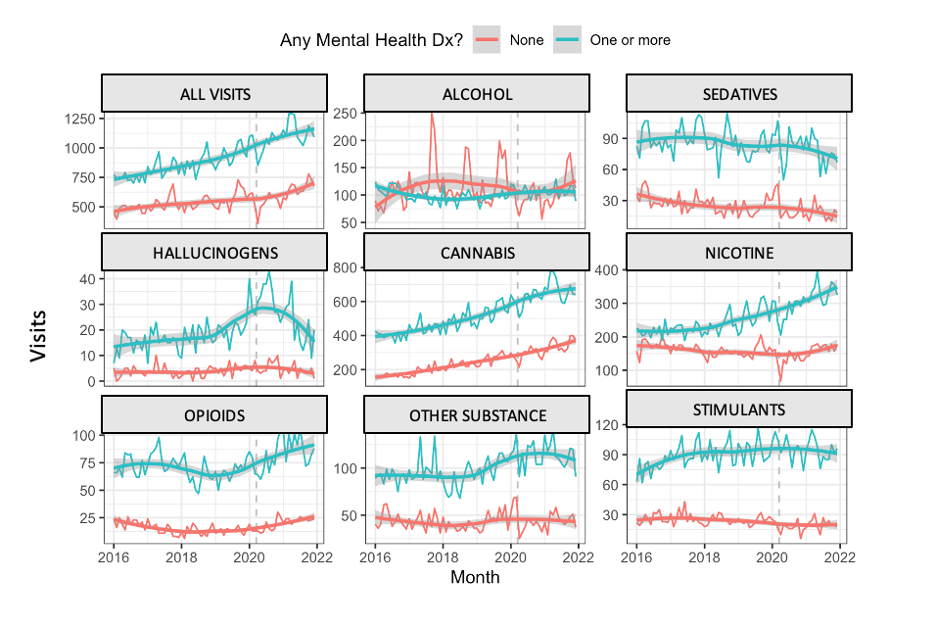
Results: Of the 106,793 total SRVs from 2016-2021, 66,980 (62.7%) involved one or more mental health comorbidity (Table 1). Top mental health comorbidities were ADHD, anxiety, depression, suicide/self injury, conduct, and trauma or stress-related disorder. Compared to those without a mental health comorbidity, SRVs with a mental health comorbidity occurred at greater frequency throughout the study for all substances except alcohol (Figure 1). There were higher odds of having any mental health comorbidity than not when presenting for all substances except alcohol and nicotine (Figure 2). The greatest odds of having any mental health comorbidity were seen among visits for opioids, hallucinogens, and polysubstance visits (aOR, 2.95 95% CI 2.76-3.15; 2.77 95% CI 2.44-3.16; 2.42 95% CI 2.33-2.51 respectively).
Conclusion(s): The mental health comorbidity for SRVs among youth has increased in children’s hospitals. SRVs with a mental health diagnosis are more common and costly than those without a mental health diagnosis. The risk is not evenly distributed and the presence of opioids or more than once substance confers some of the largest risks of having a mental health comorbidity. Greater funding and policy efforts are needed to address the increasing morbidity from adolescent substance use and mental health conditions with a focus on interdisciplinary work and increased coordination among health systems.
Characteristics of Substance-Related Visits by Mental Health Comorbidity
.png) *Interquartile range
*Interquartile rangeNumber of Visits with and without a Mental Comorbidity by Substance Type from 2016-2021
Odds of Presenting with Any Mental Health Comorbidity by Substance Type