Emergency Medicine 13
Session: Emergency Medicine 13
560 - Physician Modifiers Associated with the Evaluation of Suspected Child Physical Abuse in the Pediatric Emergency Department: A Survey Study
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 560.6112
Nikki M. Jones, Children's National Health System, Washington, DC, United States; Cassandra Colonneaux-Lee, Nemours Children's Hospital, Walton-on-Thames, England, United Kingdom; Andrea Rivera-Sepulveda, Nemours Children’s Health, Orlando, FL, United States

Nikki M. Jones, MD (she/her/hers)
General Pediatrician
Children's National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background: Child physical abuse (CPA) affects at least 1 in every 7 children in the US, accounting for significant morbidity and mortality in children less than 2 years of age. A clinical report on the evaluation of suspected CPA has been published by the American Academy of Pediatrics (AAP) have been published on the evaluation of suspected child physical abuse, stating the lasting effects of abuse, highlighting the risk factors for abuse and abusive injuries that are frequently overlooked. Medical providers in Emergency Medicine (EM) are considered frontline agents and mandated reporters who should be aware of the most updated literature on child physical abuse. However, little is known about the medical providers’ knowledge, agreement, compliance and attitudes. regarding CPA evaluation.
Objective: The objective of this study is to assess knowledge, compliance, and attitudes regarding the evaluation of suspected CPA of among Emergency Medicine medical providers.
Design/Methods: An online survey was administered among a representative sample of providers with a joint interest in PEM through the PED-EM-Listserv® and in-person at the AAP Section of Emergency Medicine at the National Conference and Exhibition in Fall 2023. The survey comprised history and physical findings associated with CPA, evaluation based on skeletal injuries, screening of occult injury, clinical vignettes, and demographics. Agreement was measured as a 5-point Likert response, and compliance was measured using diagnostic tests when faced with a clinical case.
Results: We included 228 responders, of which 53.5% identified knowing the AAP clinical report on the evaluation of CPA. There was good agreement with historical concerns for child physical abuse (α=0.796) and a high likelihood of CPA based on physical findings (α=0.809). About 82.5% of responders would further evaluate CPA in the presence of high-risk skeletal injuries. Initiation of occult injury screening was 3.8% for children < 12 months and 1% for children 12 to 24 months of age. About 93.9% of respondents had institutional clinical pathways, but only 79.4% had clinical pathways to evaluate child physical abuse.
Conclusion(s): Providers shared good agreement about the historical and physical components associated with CPA but have poor agreement in applying laboratory and radiologic studies. The assessment of providers’ knowledge and practice characteristics for the evaluation of suspected child physical abuse can help develop initiatives to improve patient care, decrease child morbidity, and standardize the identification and workup of child physical abuse in the Emergency Department.
Table 1. Demographic characteristics of participating providers (N=228).
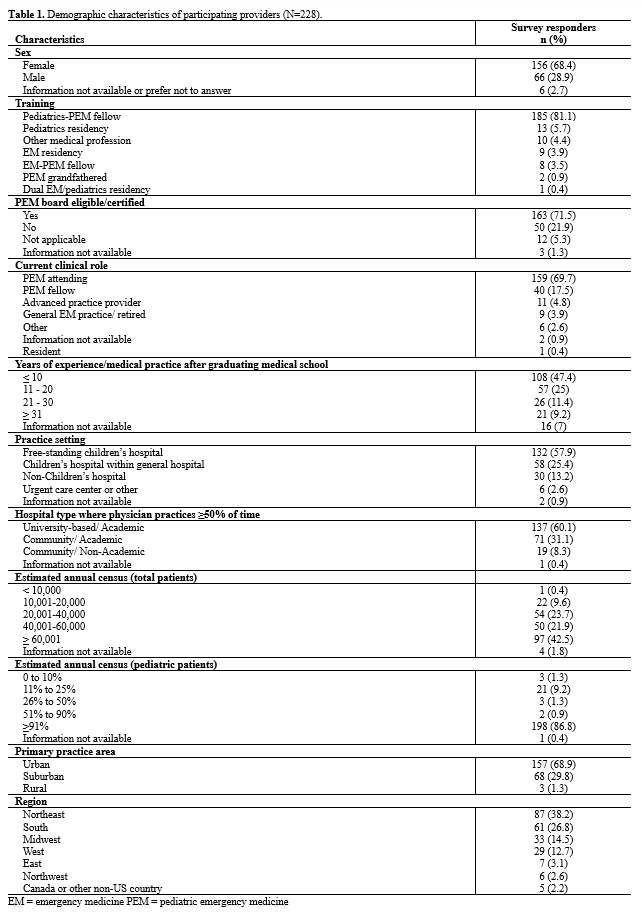 EM = emergency medicine PEM = pediatric emergency medicine
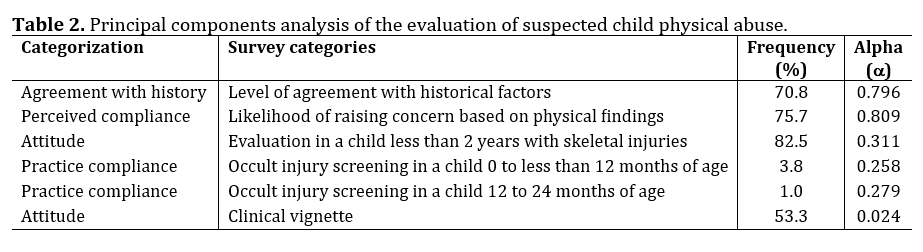
EM = emergency medicine PEM = pediatric emergency medicineTable 2. Principal components analysis of the evaluation of suspected child physical abuse.
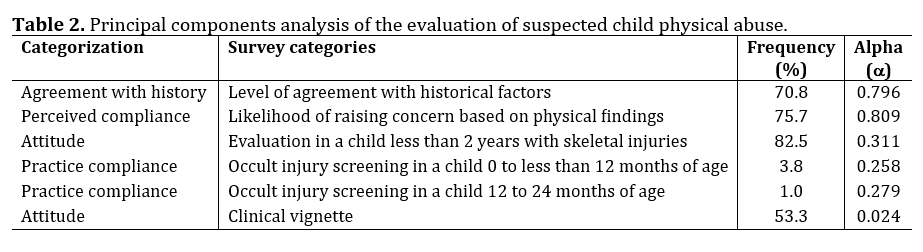
Table 1. Demographic characteristics of participating providers (N=228).
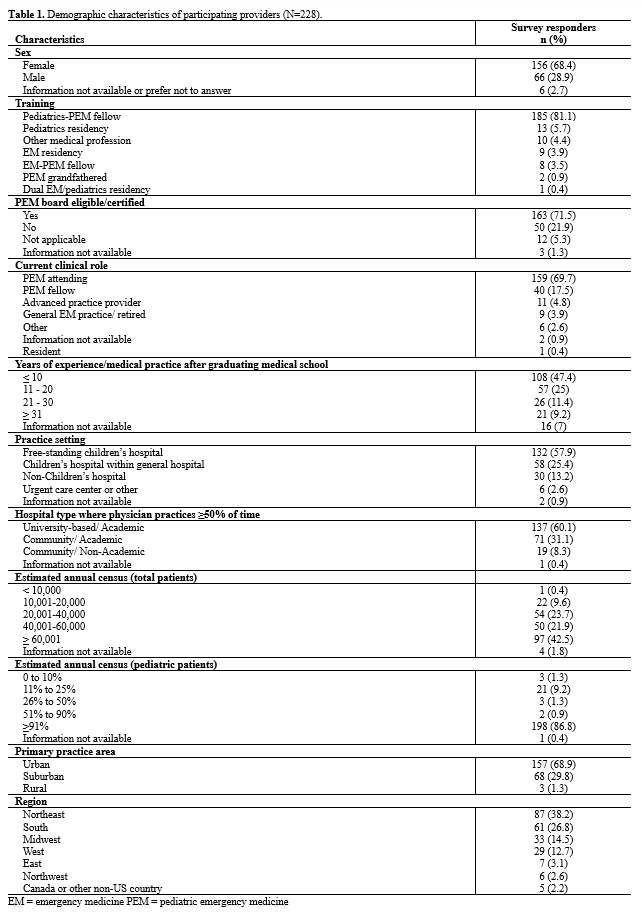 EM = emergency medicine PEM = pediatric emergency medicine
EM = emergency medicine PEM = pediatric emergency medicineTable 2. Principal components analysis of the evaluation of suspected child physical abuse.