Health Equity/Social Determinants of Health 9
Session: Health Equity/Social Determinants of Health 9
188 - Parent Preferences about AI-translated Discharge Instructions after Pediatric Hospitalization
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 188.5768
Nguyen Tran, Seattle Children's, Seattle, WA, United States; K. Casey Lion, University of Washington/ Seattle Children's Hospital, Seattle, WA, United States; Taylor Salaguinto, Seattle Children's, Seattle, WA, United States; Citlali R. Gomez Acosta, Seattle Children's Hospital, Monroe, WA, United States; Jason J. Lau, University of Washington School of Medicine, Seattle, WA, United States; Tommy Nguyen, Seattle Children's Research Institute, Seattle, WA, United States; Arti D. Desai, University of Washington School of Medicine, Seattle, WA, United States; Emily Larimer, Seattle Children's, Seattle, WA, United States; Melissa Martos, University of Washington School of Medicine, Seattle, WA, United States; Nigel Hartell, Seattle Children's, Seattle, WA, United States; Blanca Fields, Seattle Children's, Bellevue, WA, United States

Nguyen Tran, B.Sc. (he/him/his)
Clinical Research Coordinator III
Seattle Children's
Seattle, Washington, United States
Presenting Author(s)
Background: Most families who use a language other than English (LOE) for medical care do not receive language-concordant written discharge instructions, contributing to worse post-hospitalization health outcomes. Professional translation requires hours to days. Artificial Intelligence (AI) can provide translated materials for families within minutes but may also make more errors.
Objective: To understand parents' attitudes and preferences around AI translations with integrated human review.
Design/Methods: We administered a 5-question survey to a purposive sample of LOE parents of hospitalized children at a free-standing children's hospital during their stay between 8/28 – 10/29/2024. We administered the survey electronically (for Spanish) or verbally with an interpreter. The survey described the potential use of AI translation to provide language-concordant written instructions at discharge, with subsequent review and correction within 1-2 days by a professional translator as needed. Parents reported acceptability of aspects of this plan, using a 5-point Likert scale from "I dislike it" (1) to "I like it" (5), with open-ended questions to assess the rationale for their chosen response. Verbal open-ended responses were recorded verbatim, and all responses were translated into English for content analysis.
Results: Of 50 parents approached, 30 (60%) completed the survey (Table 1). Regarding the overall acceptability of AI translation for discharge instructions, 64% (19/30) selected neutral or negative responses (mean score = 2.86, SD = 1.61; Figure 1). The most frequently reported concern was the accuracy of the AI translation, citing that a computer would make more mistakes than human translators. One parent said computer-translated instructions "would make me feel unsure". 63% favored disclaimer language that AI was used during translation. When asked to choose only one approach, 43% preferred to receive written discharge instructions in English with a human-translated document 2-5 days later, and 40% of parents preferred AI-translated instructions right after the visit, with a human translator review within 1-2 days (Figure 2).
Conclusion(s): Many LOE parents of hospitalized children reported preferring accurate but delayed human translations over faster AI translations that might contain errors. This finding may contradict clinician assumptions and suggest differential levels of trust in technology, highlighting the need for parent and patient partners to guide care innovations. Ongoing data collection with this survey will increase sample size and language diversity.
Table 1. Demographics
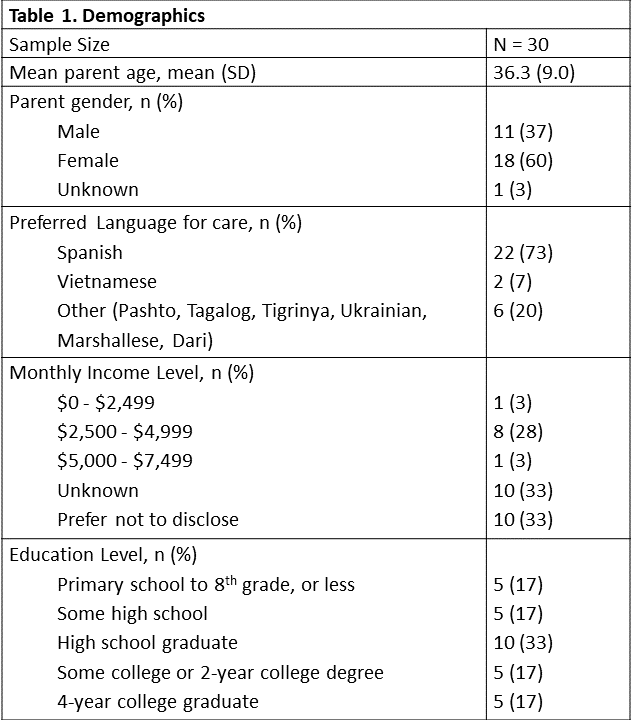
Figure 1. Parents' Responses to Attitudes and Preferences Questions
.png)
Figure 2. Parents' Preference of Instructions Post-Discharge
.png)

