Emergency Medicine 10
Session: Emergency Medicine 10
516 - Improving Time to Recognition and Management of Pediatric Sepsis in a Pediatric Emergency Department - A Quality Improvement Initiative
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 516.5133
Jennifer Jamerino-Thrush, Children's Hospital of Michigan, West Bloomfield, MI, United States; Joshua J. Green, Children's Hospital of Michigan, Detroit, MI, United States; Usha Sethuraman, Children's Hospital of Michigan, Detroit, MI, United States; Kelly Levasseur, Children's Hospital of Michigan, Detroit, MI, United States

Jennifer Jamerino-Thrush, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Children's Hospital of Michigan
West Bloomfield, Michigan, United States
Presenting Author(s)
Background: Sepsis is a leading cause of morbidity and mortality worldwide, accounting for greater than 75,000 pediatric patients treated annually in the United States. Mortality rates range from 3% to 7% in pediatric sepsis, to as high as 20% for septic shock. In children, early signs of sepsis are often subtle, which can lead to delays in recognition and treatment. Every hour of delayed treatment initiation is linked to poorer clinical outcomes.
Objective: The primary objective was to expedite the recognition of sepsis and reduce the time to intravenous fluid (IVF) bolus administration and antibiotic initiation to within 60 minutes of meeting sepsis criteria.
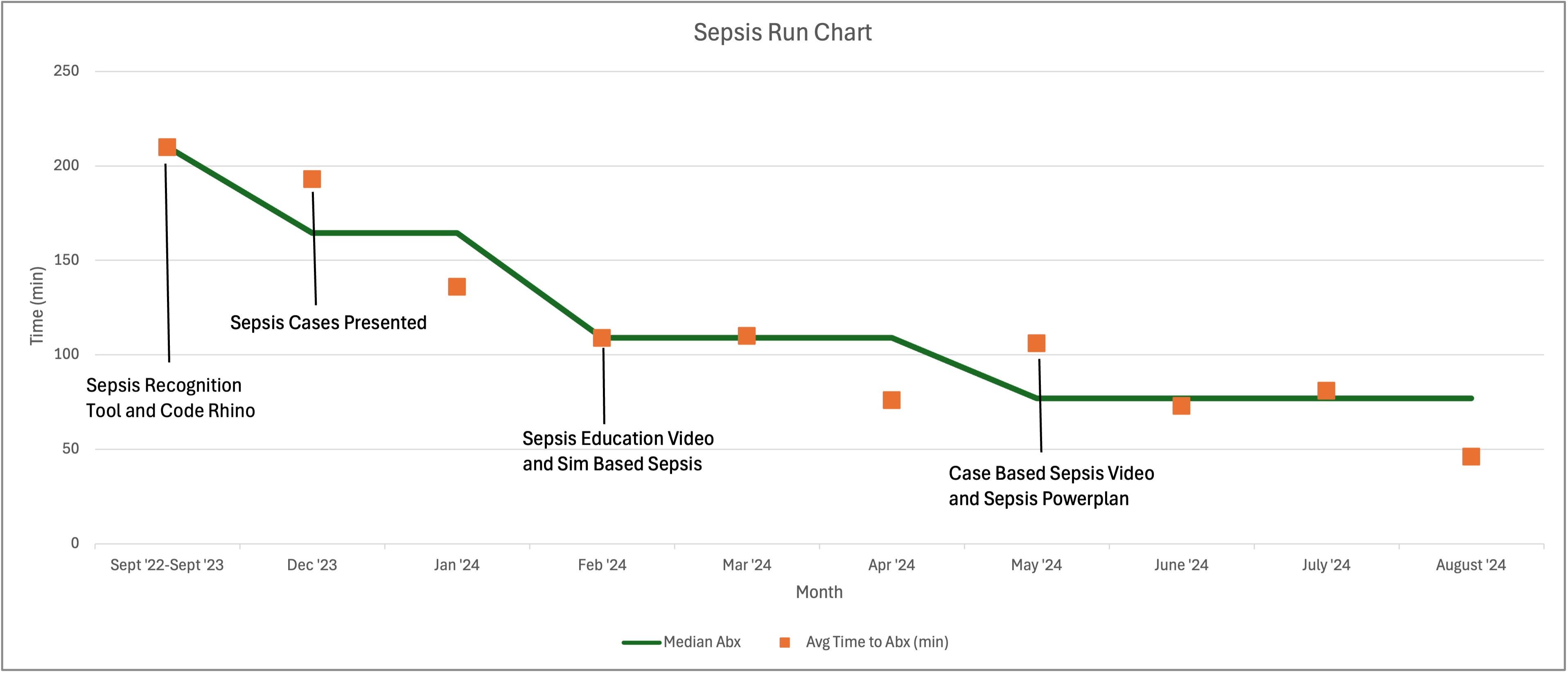
Design/Methods: A retrospective chart review was conducted on all patients with ICD codes related to sepsis who presented to the ED from September 2022 to September 2024. In September 2023, a multidisciplinary team was formed to improve the recognition and treatment of sepsis. Plan-Do-Study-Act (PDSA) cycles were implemented every 3-4 weeks from October 2023 to September 2024. Interventions included development of a sepsis recognition tool, formation of a clinical sepsis team, monthly sepsis case review, educational videos and lectures, and simulation cases for ED providers and nurses. PDSA cycles were completed following each intervention, and trends in the timing of both the first fluid bolus and initiation of antibiotics were analyzed.
Results: A total of 958 charts were reviewed of which 330 met criteria for sepsis. Each intervention contributed to a decrease in the time to both IVF bolus and antibiotic initiation. We observed a decreased time to first fluid bolus by 114 minutes (pre 153 to post 39) as well as a decreased time to antibiotics by 146 minutes (pre 210 to post 46). The most significant reduction in time to IVF bolus occurred following implementation of the sepsis recognition tool and the formation of the clinical sepsis team resulting in a 39-minute decrease in mean time. While the most significant reduction in time to antibiotics occurred after the introduction of monthly sepsis case review, with a 57-minute decrease in mean time.
Conclusion(s): This quality improvement initiative demonstrates a significant decrease in both time to IVF bolus and antibiotics by utilizing a multidisciplinary approach and focusing on timely identification and intervention of sepsis. Future efforts will focus on sustaining these improvements and spreading best practices to other hospital departments.
Time to IV Fluids Run Chart
.png)
Time to Antibiotics Run Chart
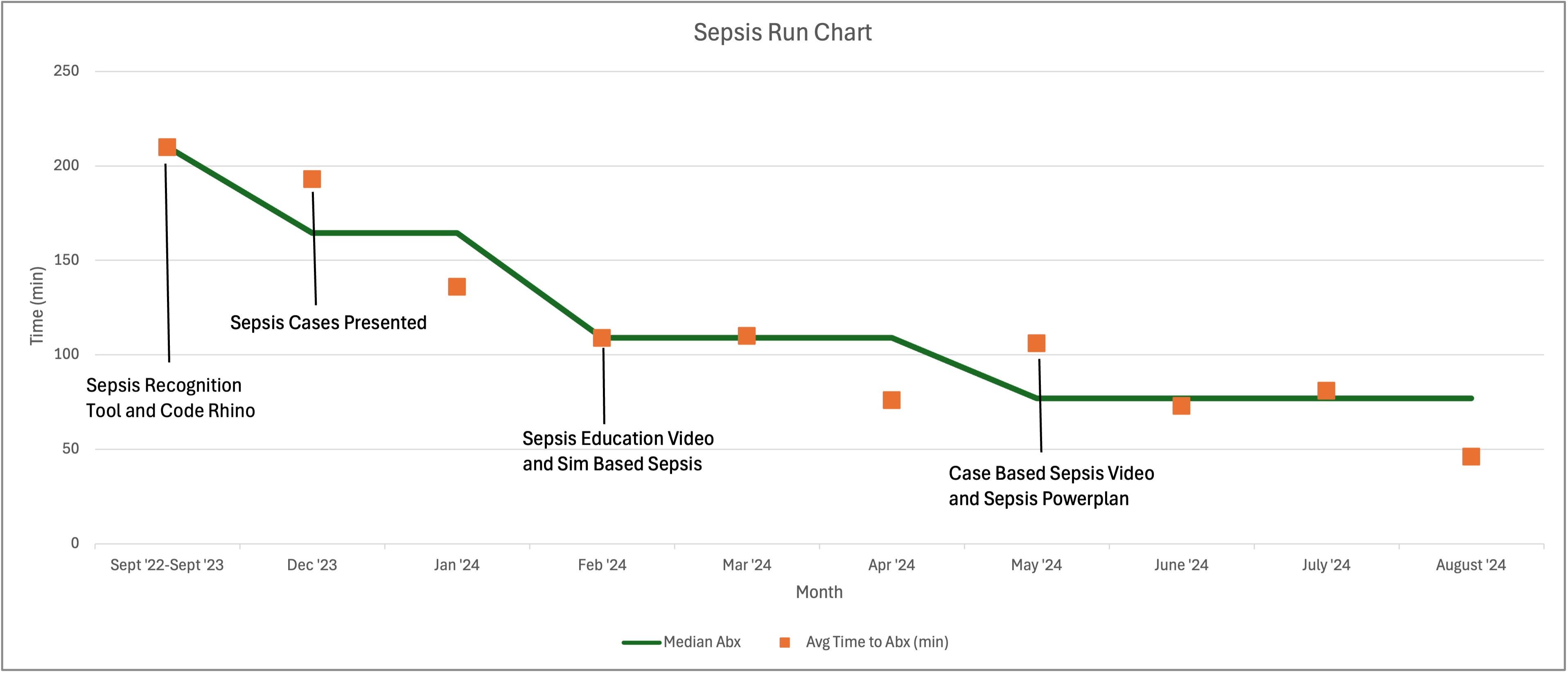
Time to IV Fluids Run Chart
.png)
Time to Antibiotics Run Chart