Emergency Medicine 14
Session: Emergency Medicine 14
578 - Using Quality Improvement Methodology to Reduce Length of Stay for Patients with Simple, Isolated Lacerations in the Pediatric Emergency Department (PED)
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 578.7121
Emily A. Kleiman, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Christopher M.. Pruitt, Medical Director, Pediatric Emergency Medicine, MUSC Children's Health, Charleston, SC, United States; Barron Frazier, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States

Emily A. Kleiman, MD (she/her/hers)
Pediatric Emergency Medicine Fellow
Medical University of South Carolina College of Medicine
Charleston, South Carolina, United States
Presenting Author(s)
Background: Lacerations are among the most common presenting complaint in the PED. Many are repaired by the emergency provider; however, lengths of stay (LOS) for these patients often do not accurately reflect the short duration of time actually required for repair. Prolonged LOS is associated with crowding, which is well established as a significant barrier to providing safe and high quality care in the PED setting.
Objective: To reduce provider-to-discharge time by 20% within 12 months using bundled intervention strategies centered around modifiable delays of care for patients with isolated, simple lacerations.
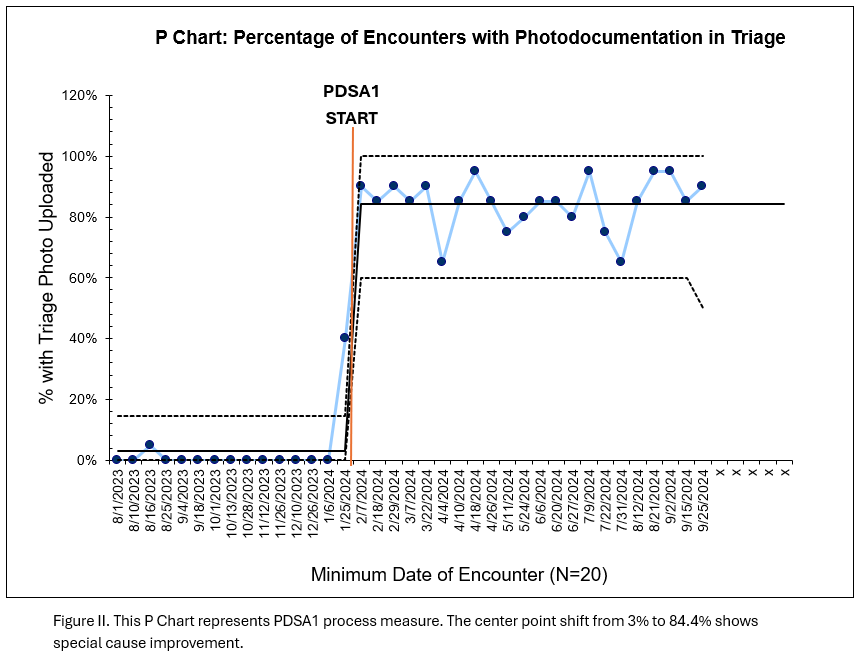
Design/Methods: The Model for Improvement with sequential PlanDoStudyAct (PDSA) cycles was used to achieve project aims. A root cause analysis and key driver diagram identified barriers to care. Interventions centered around standardizing the triage process and addressed several key drivers: time to analgesia/anxiolysis, time to provider evaluation/plan, caregiver involvement, standing order use, and provider comfort with evidence-based practice. In PDSA1, we introduced a novel triage process for all lacerations: nurse photographs laceration, uploads image to the patient’s medical chart, then uses a standing order to immediately apply topical anesthetic to the wound. Analysis included all patients with isolated lacerations. We excluded patients if: any consult order was placed, procedural sedation used, imaging ordered, or patient received >2 medications from inpatient pharmacy during the encounter. Primary outcome was time from first provider evaluation to discharge in minutes. Data was analyzed with X-bar/S control and P charts. We used established rules to detect special cause. Demographic data pre- and postintervention were compared using t tests and Mann-Whitney tests.
Results: Seven hundred thirty patients were included, 292 pre-and 438 postintervention. There was no statistically significant difference between patient age, gender, laceration location, and repair type between the two groups (Table I). We reduced the average time from provider evaluation to discharge from 84.9 minutes to 66.8 minutes (21.3% reduction) during the study period (Figure 1). This has been sustained for 7 months at time of abstract submission. The percentage of patients with photodocumentation was used as a process measure and is represented by a P chart (Figure 2). All process measures showed special cause improvement.
Conclusion(s): A quality improvement process to optimize triage of children with lacerations led to sustained improvement in patient throughput in our emergency department.
Table I: Patient Demographics
.png)
Figure I: X-bar / S control chart: Time from First Provider Evaluation to Discharge for Patients with Isolated Lacerations in a Pediatric Emergency Department
.png)
Figure II. P Chart: Percentage of Encounters with Photodocumentation in Triage