Emergency Medicine 11
Session: Emergency Medicine 11
533 - Unlocking Prognostic Potential: Biomarker Predictors of Admission and Length of Stay in Pediatric Sickle Cell Vaso-Occlusive Pain Crisis
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 533.6537
Jeffrey Hernandez, St. Christopher's Hospital for Children, Philadelphia, PA, United States; Abhishek Dutta, St. Christopher's Hospital for Children, Philadelphia, PA, United States; Luis L. Gamboa, Drexel University College of Medicine, Philadelphia, PA, United States; Nataly Apollonsky, St.Christopher's hospital for Children, Philadelphia, PA, United States; Bruce A. Bernstein, Jefferson University: College of Population Health, Mansfield Center, CT 06250, CT, United States; Jacob W. Lowry, Drexel University College of Medicine, Gibsonia, PA, United States
.jpg)
Jeffrey Hernandez, M.D (he/him/his)
Resident Physician
St. Christopher's Hospital for Children
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Vaso-occlusive pain crisis (VOC) is the most common complication and the hallmark of Sickle Cell Disease (SCD), often necessitating hospitalization and resulting in prolonged length of stay (LOS) in pediatric patients. Predicting the severity and duration of VOC episodes remains challenging, hindering optimal management strategies. Biomarkers have emerged as potential predictors of disease severity and prognosis in various medical conditions, yet their utility in predicting admission rates and LOS in pediatric SCD patients during VOC episodes remains unclear.
Objective: This study aims to investigate biomarkers as predictors of hospital admission and LOS in pediatric patients with SCD experiencing VOC presenting to St. Christopher’s Children Hospital Emergency Department (SCHC ED).
Design/Methods: This was a retrospective chart review study of patients with SCD (all genotypes) presenting to a Level I Pediatric Trauma Center with VOC and admitted between January 1, 2019 and April 30, 2024. Data collected included demographical information (age, gender, race/ethnicity), clinical characteristics (sickle cell disease genotype), disease modifying therapies (hydroxyurea, chronic PRBC transfusions, Adakveo), vital signs obtained from the ED (oxygen saturation and blood pressure), laboratory investigations obtained from most recent outpatient hematology clinic visit and ED (particularly white blood cell count, hemoglobin, platelet count, absolute neutrophil count, reticulocyte count), and total length of hospital stay. Regression analyses were performed to assess the association between biomarker levels and the primary outcomes (inpatient admission and length of stay). ROC curve analysis was conducted to determine predictive performance of biomarkers for hospital admission and length of stay. Statistical analyses such as independent samples t-tests or chi square were conducted to explore group differences.
Results: A total of 100 patients were included in the study. There was a significant relationship (r = .242, p = .015) between systolic blood pressure at admission and length of stay. There was a significant negative correlation (r = - .217, p = .031) between admission hemoglobin and length of stay when controlling for steady state hemoglobin.
Conclusion(s): Higher systolic blood pressures and lower hemoglobin levels at the time of admission were associated with a prolonged LOS. Further investigation is warranted to gather biomarker data across multiple admissions for each patient to fully elucidate the significance of our findings.
Table 1. Demographics, SCD Genotype, and LOS
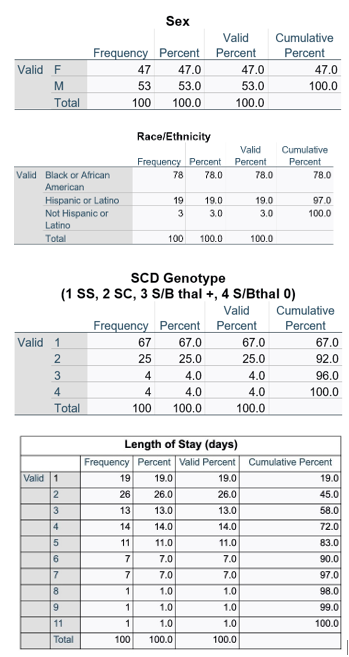
Table 2. Pearson Correlations
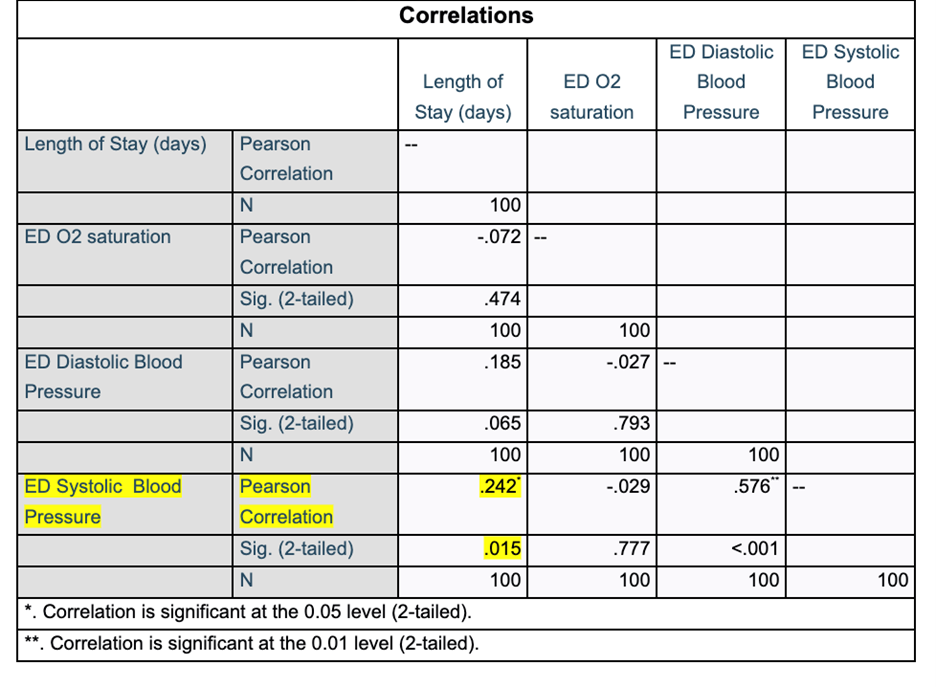
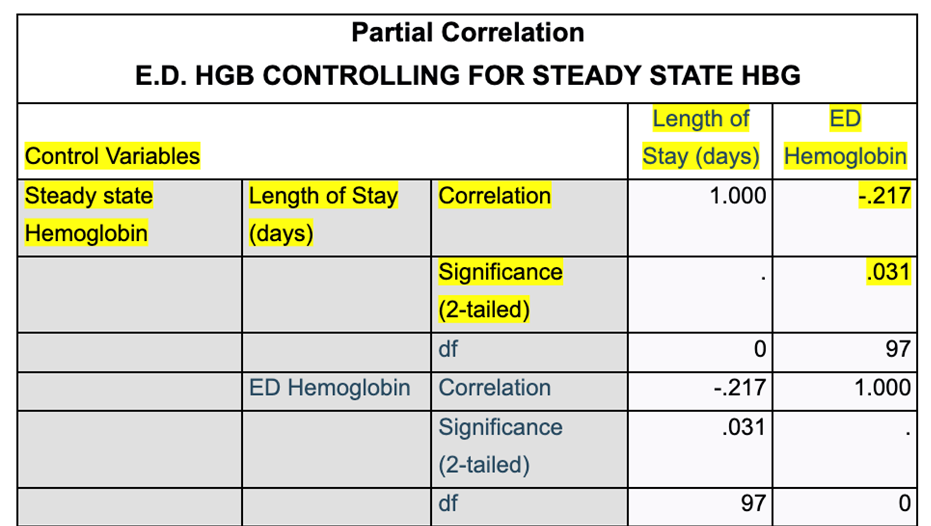
Table 3. Partial Correlations
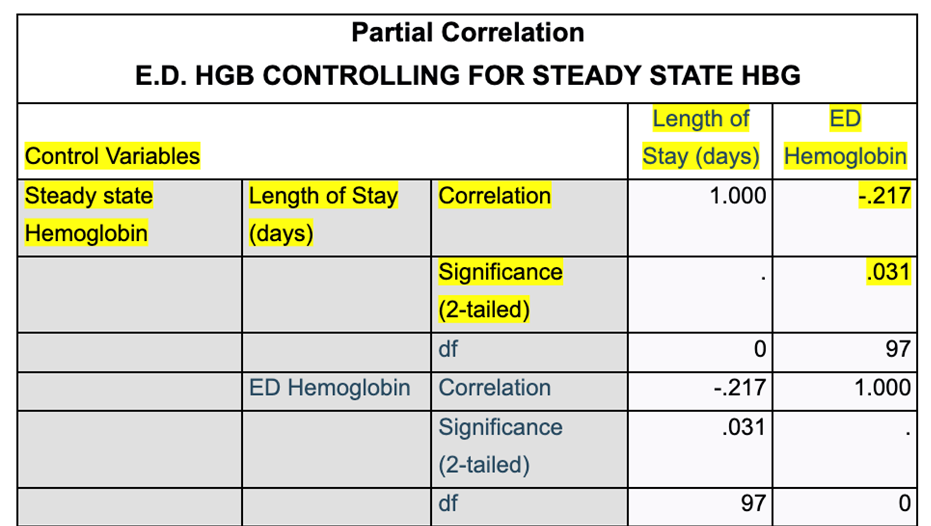
Table 1. Demographics, SCD Genotype, and LOS
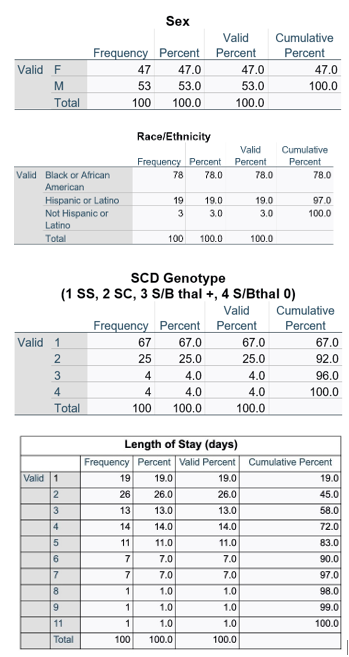
Table 2. Pearson Correlations
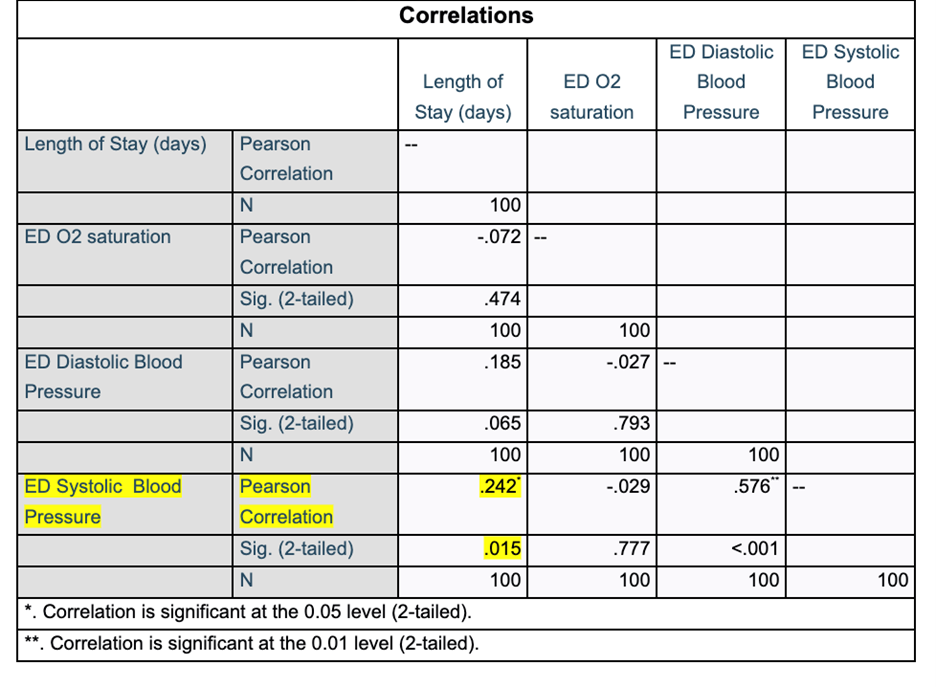
Table 3. Partial Correlations