Emergency Medicine 11
Session: Emergency Medicine 11
531 - Status of State Trauma Registries 2024: Have we made progress?
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 531.6565
Elizabeth Lendrum, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Haley Hayes, Cincinnati Children's Hospital Medical Center, West Chester, OH, United States; Meera Kotagal, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Brad Sobolewski, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; David Schnadower, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States

Liz Lendrum, MD (she/her/hers)
Clinical Fellow
Cincinnati Children's Hospital Medical Center
Cincinnati, Ohio, United States
Presenting Author(s)
Background: High-quality, granular, accessible, and timely data are essential for understanding trauma ecosystems and implementing programs to improve trauma care. State trauma registries play a crucial role in collecting, disseminating, and sharing data for researchers, implementation scientists, and policymakers.
Objective: To assess the current status and progress of statewide trauma registries over the past 20 years, with a specific emphasis on pediatric data quality, and identify opportunities for improvement.
Design/Methods: A structured electronic survey was administered to eligible and consenting state trauma registry managers between July 2024 and November 2024. The survey collected information on registry infrastructure, data collection and reporting processes, data quality assurance measures, and specific pediatric data criteria. Summary data for each state were compiled and reviewed for accuracy by the respondents. Findings were compared with those from a similar survey conducted in 2004.
Results: All 50 states and the District of Columbia participated in the survey. Forty-seven (92%) states reported active trauma registries, an increase of 15 since 2004 (Figure 1). Four states have never had a state trauma registry; however, two of those states are planning registry development. Among states with registries, 11(22%) mandate data submission from all hospitals. While many registries have transitioned to web-based systems and updated software over the last 20 years, 34 registries (67%) still rely on manual data abstraction, and most lack integration with electronic medical records (31, 61%). Furthermore, fewer than half of the state registries (20, 39%) contribute data to national collection efforts. Although most registries include designated pediatric trauma centers with pediatric age patients (37, 73%), 31 registries (61%) do not have inclusion criteria that are specific to pediatric trauma patients.
Conclusion(s): While progress has been made in establishing state trauma registries since 2004, there are glaring deficiencies, particularly in the reliance on manual data entry, the lack of integration with electronic medical records and the paucity of pediatric specific criteria. Addressing these deficiencies is essential for providing accurate, actionable, and timely data to clinicians, researchers, implementation scientists, and policy makers.
Figure 1: Status of State Trauma Registries
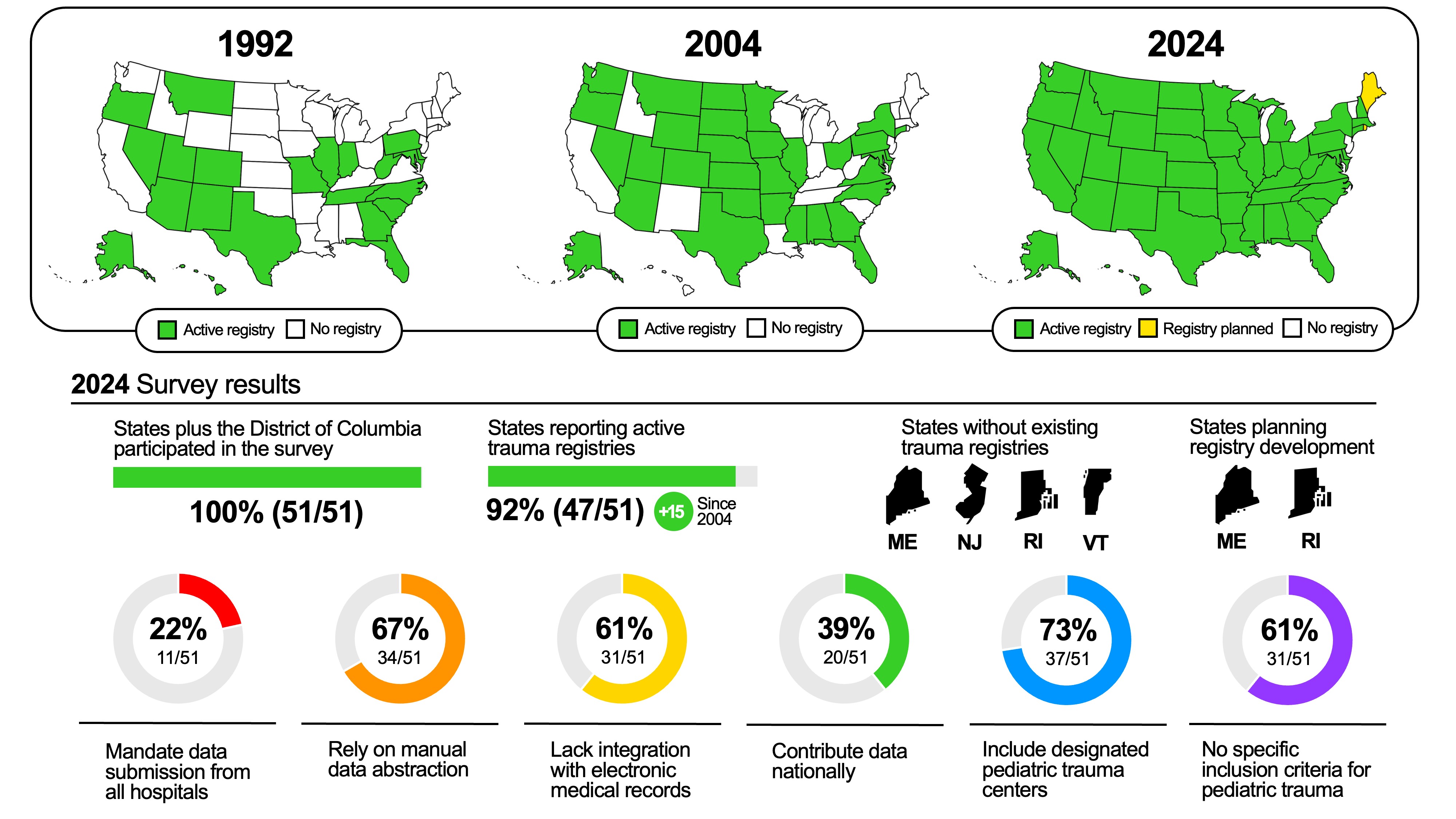 This infographic displays a summary of the status of statewide trauma registries.
This infographic displays a summary of the status of statewide trauma registries. Figure 1: Status of State Trauma Registries
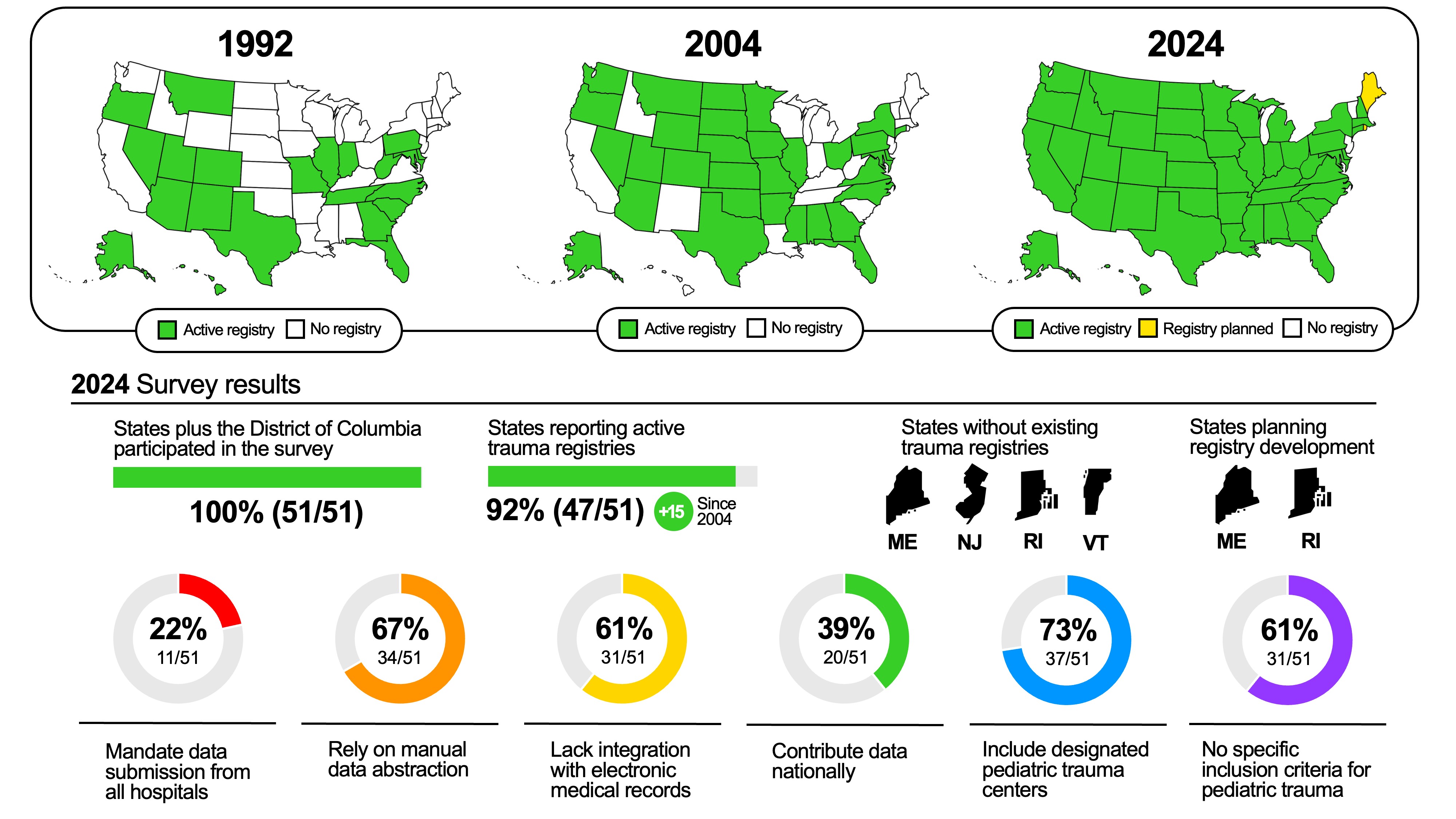 This infographic displays a summary of the status of statewide trauma registries.
This infographic displays a summary of the status of statewide trauma registries. 
