Emergency Medicine 14
Session: Emergency Medicine 14
574 - Real-World Effectiveness of Intranasal Midazolam for Procedural Anxiety in the Emergency Department: Incidence of Nonresponse during Laceration Repair
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 574.6281
Sarah R. Martin, University of California, Irvine, School of Medicine, Irvine, CA, United States; Kelly Bauer, University of California, Irvine, School of Medicine, Dana Point, CA, United States; Theodore Heyming, CHOC Children's Hospital of Orange County, Orange, CA, United States; Jenny R. Zhu, CHOC Children's Hospital of Orange County, Orange, CA, United States; Helen Lee, CHOC Children's Hospital of Orange County, Orange, CA, United States; Zeev Kain, University of California, Irvine, School of Medicine, Newport Coast, CA, United States
.jpeg.jpg)
Sarah R. Martin, PhD (she/her/hers)
Assistant Professor
University of California, Irvine, School of Medicine
Irvine, California, United States
Presenting Author(s)
Background: Pediatric laceration repairs are common in the emergency department (ED) and often associated with significant procedural anxiety. The use of intranasal midazolam (INM) prior to pediatric ED procedures has increased in recent years and, although existing evidence indicates that INM is a safe and efficacious sedative premedication, there is limited real-world evidence specifically examining the effectiveness of INM on procedural anxiety in the ED.
Objective: This study aimed to describe the proportion of children who were nonresponsive to INM (i.e., exhibited extreme anxiety) and identify factors associated with INM non-response.
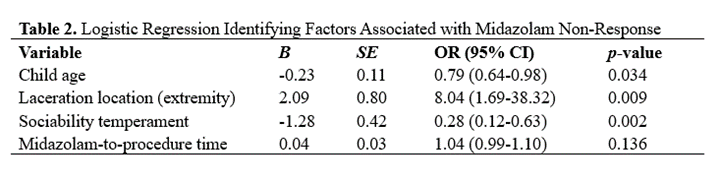
Design/Methods: This cross-sectional study included children, ages 2–10 years, who received INM prior to laceration repair in the ED. Procedural anxiety was assessed via video data using the modified Yale Preoperative Anxiety Scale (mYPAS). Children exhibiting extreme procedural anxiety (mYPAS score >72.91) when procedure started were labeled as INM non-responders. Clinical procedures and INM dosing (0.2 mg/kg) followed the institution’s standard of care guidelines. Bivariate and multivariable logistic regression analyses explored associations between child age, temperament, laceration location, time from INM administration, and likelihood of INM nonresponse.
Results: In a sample of 102 children (Mean Age±SD=4.71±2.17, 40% female, 62% Latinx), 45.1% were classified as INM nonresponders, exhibiting extreme procedural anxiety. Bivariate analyses indicated that nonresponders were younger (Z=-1.96, p=.050), had lower sociability temperament (Z=-2.77, p=.006), longer delay between INM administration and procedure (Z=-2.10, p=.035), and were more likely to have extremity lacerations (X2=8.65, p.003). In the logistic regression, younger age (OR=0.79 95%CI[0.64,0.98), lower sociability temperament (OR=0.28 95%CI[0.12,0.63]), and extremity lacerations (OR=8.04 95%CI[1.69,38.32]) were significantly associated with likelihood of INM nonresponse (p’s <.05).
Conclusion(s): Nearly half of the children in this sample exhibited extreme procedural anxiety despite receiving INM. The high incidence of nonresponse to INM has important clinical practice implications and suggests that pharmacological interventions alone may not be sufficient to manage all pediatric procedural anxiety in the ED. Findings highlight a need for further research examining multimodal strategies to manage procedural anxiety in the pediatric ED, particularly for younger children with low sociability temperament or extremity lacerations.
Table 1. Proportion of Midazolam Responders and Non-Responders Across Study Variables
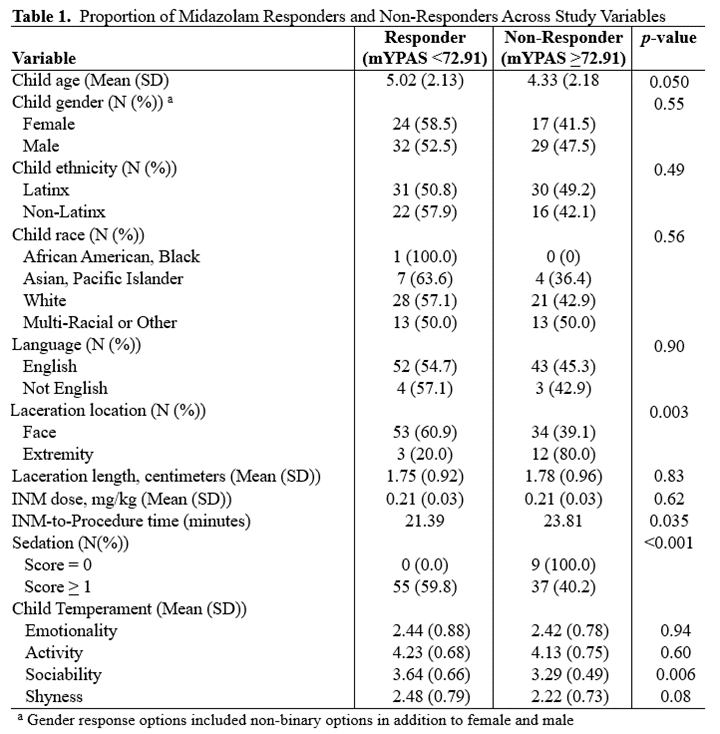
Table 2. Logistic Regression Identifying Factors Associated with Midazolam Non-Response