Emergency Medicine 4
Session: Emergency Medicine 4
253 - Rethinking Pediatric TBI Management: The Impact of Institution-Specific Modified Brain Injury Guidelines on Safety and Costs
Saturday, April 26, 2025
2:30pm - 4:45pm HST
Publication Number: 253.6260
Justine Lam, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Nathaniel Roddenberry, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Denes Szekeres, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Korry .. Wirth, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Katherine Riera, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Nicole A.. Wilson, Golisano Children's Hospital at The University of Rochester Medical Center, Rochester, NY, United States
- JL
Justine Lam, B.S. (she/her/hers)
Master's Student
University of Rochester School of Medicine and Dentistry
Rochester, New York, United States
Presenting Author(s)
Background: Traumatic brain injury (TBI) incurs high healthcare costs, largely due to resource-intensive management that does not account for varying injury severity. We developed institution-specific modified brain injury guidelines (RmBIG) based on published guidelines and consensus of involved services.
Objective: To retrospectively evaluate the theoretical safety, resource utilization, and cost savings associated with RmBIG implementation in pediatric patients with TBI. We hypothesize that RmBIG implementation will enhance efficiency and reduce costs without compromising safety in pediatric patients with mild-to-moderate TBI.
Design/Methods: After IRB approval, we retrospectively reviewed all children (age < 18y) with acute TBI who required a trauma team activation (1/2014-12/2021) using our institutional trauma registry and electronic medical record. Patients lacking head CT or other necessary data were excluded (Figure 1). Patients were categorized by TBI severity (RmBIG1-3; Table 1). Safety was evaluated based on guideline category upgrades, while resource utilization focused on potential reductions in repeat CTs and hospital/ICU admissions.
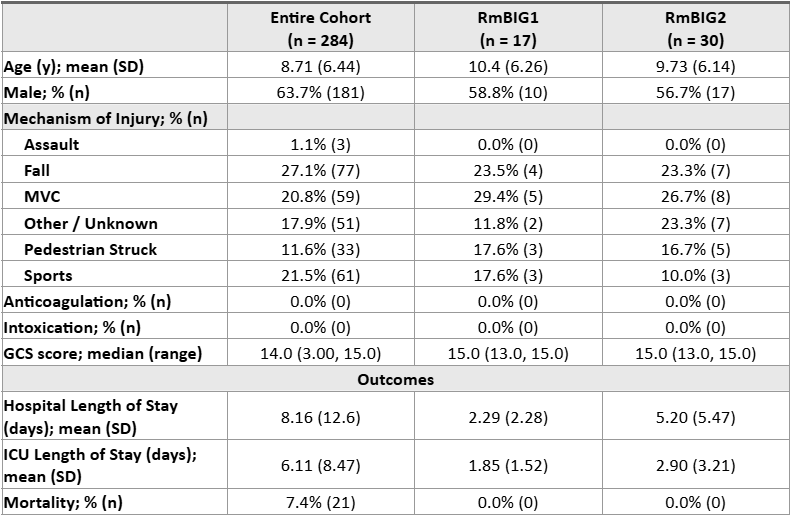
Results: Of 284 patients, 6.0% (17) had mild TBI (RmBIG1), 10.6% (30) moderate (RmBIG2), and 83.4% (237) severe (RmBIG3). Overall, the mortality rate was 7.4% (21), but 0% in RmBIG1 and RmBIG2 (Table 2). No RmBIG1 patients required a guideline category upgrade, while 2 (6.7%) RmBIG2 patients progressed to RmBIG3. The mean (SD) number of head CTs per patient was 1.18 (0.39) for RmBIG1 and 1.53 (0.78) for RmBIG2. RmBIG implementation would have prevented 3 repeat head CTs for RmBIG1, saving $3,828 ($1,276 per CT). Although potentially driven by other injuries, ICU admissions would be reduced by approximately 36.63 ICU days, saving $219,780 (~$6,000 per ICU-day). For example, of the 6 RmBIG1 patients with ICU admissions, 1 had other injuries requiring ICU admission, 4 required only floor admission for other injuries or social concerns, and 1 could have been observed in the ED.
Conclusion(s): Our results demonstrate that TBI management is not perfectly adapted to varying injury severity. RmBIG implementation will improve care standardization and resource utilization without compromising safety in pediatric patients with mild-to-moderate TBI. While hospital and ICU days are expected to decrease with RmBIG implementation, lengths of stay can be driven by other injuries and/or social concerns. We plan to perform a prospective study to coincide with RmBIG implementation, which will address this concern.
Figure 1. Patient Inclusion and Exclusion Flowchart
.png)
Table 1. RmBIG Criteria Description.
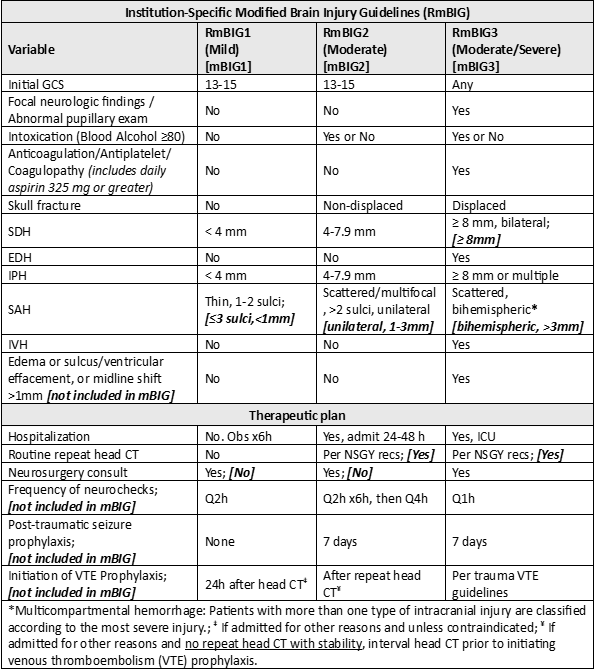 In places where the institution-specific guidelines deviate from existing modified brain injury guidelines (mBIG)6,7, the relevant mBIG criteria are shown in brackets.
In places where the institution-specific guidelines deviate from existing modified brain injury guidelines (mBIG)6,7, the relevant mBIG criteria are shown in brackets.Table 2. Patient Demographics, Injury Characteristics, and Outcomes.