Neonatal GI Physiology & NEC 3
Session: Neonatal GI Physiology & NEC 3
696 - Predicting Infection Risk in Infants with Gastroschisis
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 696.6396
Alaina Pyle, Connecticut Children's Medical Center, University of Connecticut School of Medicine, MONROE, CT, United States; Isabella Zaniletti, IZ Statistics LLC, Tampa, FL, United States; Theresa Grover, University of Colorado School of Medicine, Aurora, CO, United States; Elizabeth N. Jacobson, University of Washington, Seattle, WA, United States; Heidi E. Karpen, Emory University School of Medicine, Atlanta, GA, United States; Karna Murthy, Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, United States; Michael A. Padula, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Stefanie Riddle, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Franscesca Miquel-Verges, University of Arkansas for Medical Sciences, Little Rock, AR, United States

Alaina Pyle, MD
Attending Neonatologist
Connecticut Children's Medical Center, University of Connecticut School of Medicine
MONROE, Connecticut, United States
Presenting Author(s)
Background: Infants with gastroschisis require prolonged inpatient care due to sequelae that include feeding intolerance, risk of intestinal failure, and courses which are often complicated by postnatal infections. Though multiple mechanisms of incident infections may exist in these affected infants, criteria defining which patients are at highest risk remain uncertain.
Objective: To estimate the associations between clinical factors and incident bloodstream (BSI) and urinary tract infections (UTI) in infants with gastroschisis.
Design/Methods: We conducted a retrospective analysis using the Children’s Hospitals Neonatal Database (CHND) from 2010-2023, assessing infants with gastroschisis from North American neonatal intensive care units (NICUs). Centers that contributed < 30 cases were omitted. The main outcomes were culture-positive BSI or UTI during the NICU hospitalization. Multivariable logistic regression models were used to determine clinical, demographic, and practice-based variables associated with the main outcomes. Odds ratios (OR) and 95% confidence intervals (CI) are reported.
Results: From 31 hospitals, there were 3,987 infants with gastroschisis; 302 (7.6%) had BSI and 141 (3.5%) had UTI, and 22 (0.5%) had both within 48 hours of each other. Gestational age was similar across groups (36 weeks), as was male sex (51.1%), with predominantly non-Hispanic white race/ethnicity (53.6%). Sepsis on admission was rare (0.35%). The mean age at BSI was 43.2 days (SD 42.2), and mean age at UTI was 47.9 days (SD 34). In both unadjusted and multivariable analyses, incident BSI was associated with bowel atresia, necrotizing enterocolitis or intestinal perforation, patch closure, congenital heart disease, silo/staged closure, and patch closure (Table 1). Incident UTI is independently associated with gestational age, SGA < 10th centile, genitourinary anomaly, bowel atresia, sutureless closure and patch closure (Table 2). These models performed modestly for both BSI (AUC = 0.66) and UTI (AUC=0.71).
Conclusion(s): Among infants with gastroschisis, clinical variables can be used to risk-stratify infants for incident infection. The risk may be predicted by markers of complex forms of gastroschisis, such as bowel atresia, NEC/perforation, and patch use. Applying these results suggest novel methods to improve antibiotic stewardship efforts and reduce antibiotic overuse in affected infants.
Table 1: Multivariable Analysis, Main outcome of BSI in infants with Gastroschisis
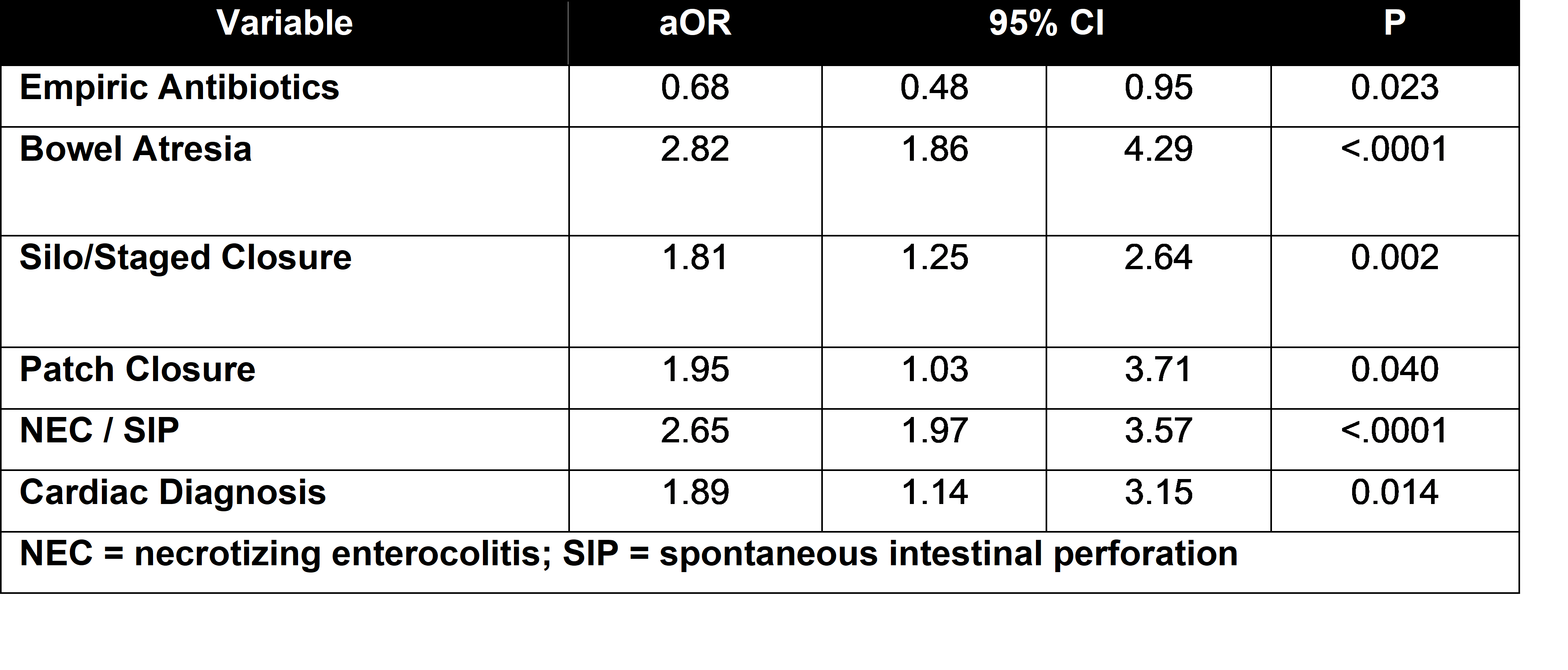
Table 2: Multivariable Analysis, Main outcome of UTI in infants with Gastroschisis
.png)

