Medical Education 13: Potpourri
Session: Medical Education 13: Potpourri
278 - Perspectives of the Advanced Practice Provider's Role in Physician Medical Education: Current State and Future Direction
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 278.6395
Alexandra Comfort, University of Utah School of Medicine, Sandy, UT, United States; Jennifer Berger, University of Nebraska College of Medicine, Omaha, NE, United States; Deborah DiazGranados, Virginia Commonwealth University School of Medicine, Richmond, VA, United States; Debra Shockey, Virginia Commonwealth University, Richmond, VA, United States; Alanna Higgins Joyce, Northwestern University The Feinberg School of Medicine, Chicago, IL, United States; Chris B. Peltier, Cincinnati Children's Hospital Medical Center, South Lebanon, OH, United States; Nathan S. Gollehon, Omaha Children's Hospital, Elkhorn, NE, United States; Marieka Helou, Virginia Commonwealth University School of Medicine, Richmond, VA, United States

Alexandra Comfort, MD (she/her/hers)
Resident
University of Utah School of Medicine
Sandy, Utah, United States
Presenting Author(s)
Background: Advanced practice provider (APP) and physician learner interactions are increasing at academic medical centers (AMC) due to duty hour restrictions, changes in billing requirements, and new residency program requirements. However, limited studies evaluate the overall quality of APP supervision and evaluation. While perceptions vary, it is clear the APP role in physician education has not been formalized.
Objective: We conducted a stakeholder survey to 1) describe current interactions and 2) compare perceptions of the potential APP role.
Design/Methods: Four anonymous surveys were designed for each stakeholder group: medical students (MS), residents, faculty, and APPs working in pediatric departments. The surveys consisted of 2 domains to explore each of our aims. Surveys were distributed via email listservs at participating AMCs and included an incentive upon completion. Questions were compared across stakeholder groups using chi-square tests with Bonferroni-adjusted p-values.
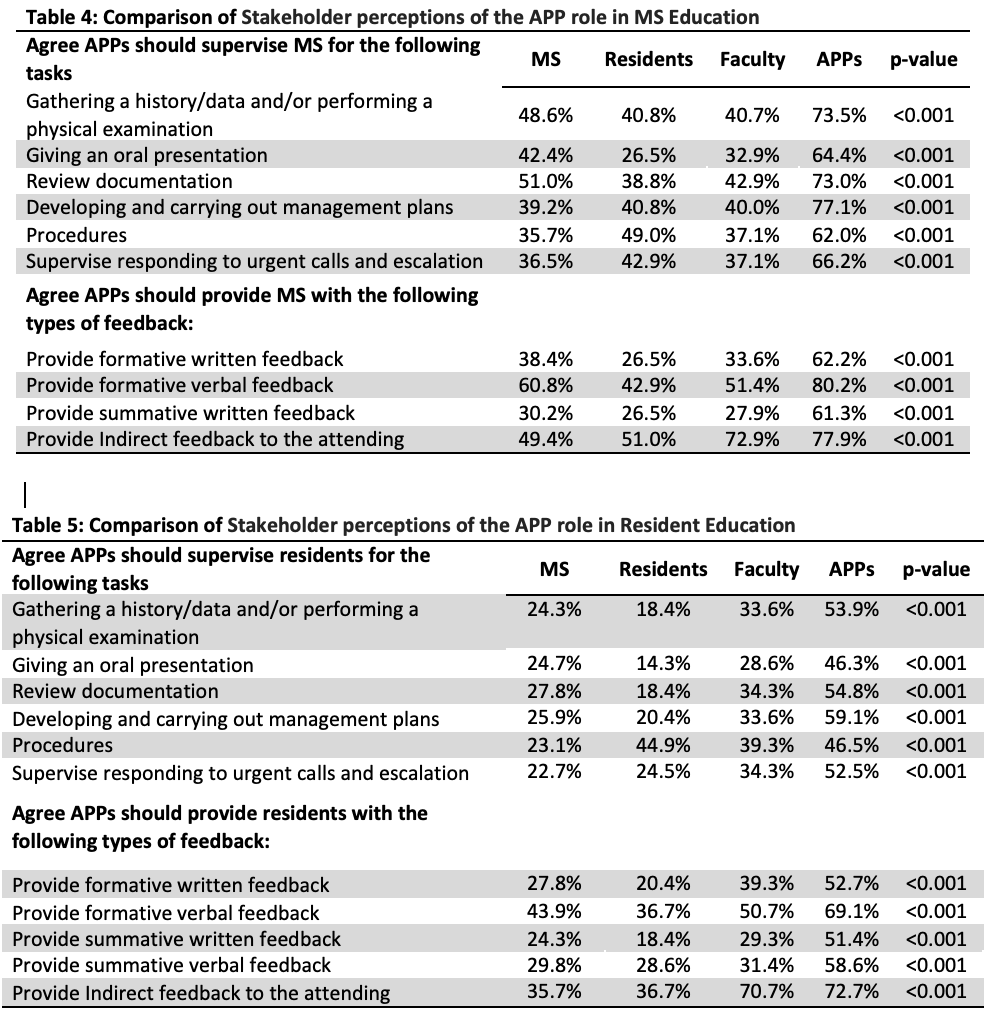
Results: Survey respondents are described in Table 1. For the 1st domain, frequency of supervision for specific tasks and type of feedback are provided in Tables 2 and 3. Of note, for resident tasks supervised, most residents and faculty reported procedures compared to only a third of APPs. For type of feedback, most MS and APPs both reported formative verbal compared to only a third of faculty. For resident feedback, most faculty reported indirect feedback to the attending compared to only a third of residents and APPs. The second domain of questions on the potential APP role are compared in Tables 4 and 5. For all tasks, APPs were more likely to agree they should supervise both MS and residents than any other group. APPs were also more likely to agree that they should provide all types of feedback/evaluation with faculty agreeing with indirect feedback only (p-values < 0.001).
Conclusion(s): Our study reveals varying perceptions of the APP role in physician training, with APPs generally believing they currently do and should supervise most tasks and provide most types of feedback. However, MS, residents, and faculty do not appear to share this viewpoint. At best, this difference of opinion could cause dissatisfaction with the learning environment and at worst, lead to tension and poor communication, acting as an obstacle to patient care. It is crucial that we take a closer look at the root causes for this discord. Our survey included free text comments which are being analyzed for themes as well as to inform future qualitative studies. This work could be the first step in guiding policy on the APP role in physician medical education.
Table 1: Summary of Respondents; Table 2: Descriptive statistics of the MS/APP experience at current state^
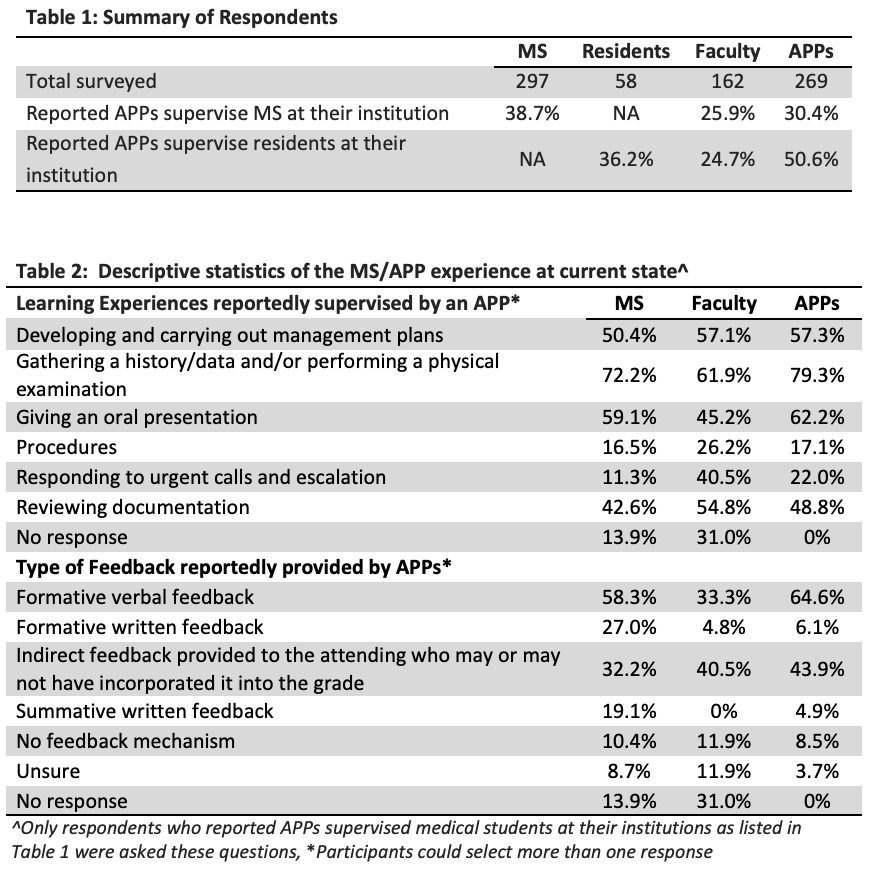
Table 3: Descriptive Statistics of the resident/APP experience at current state^
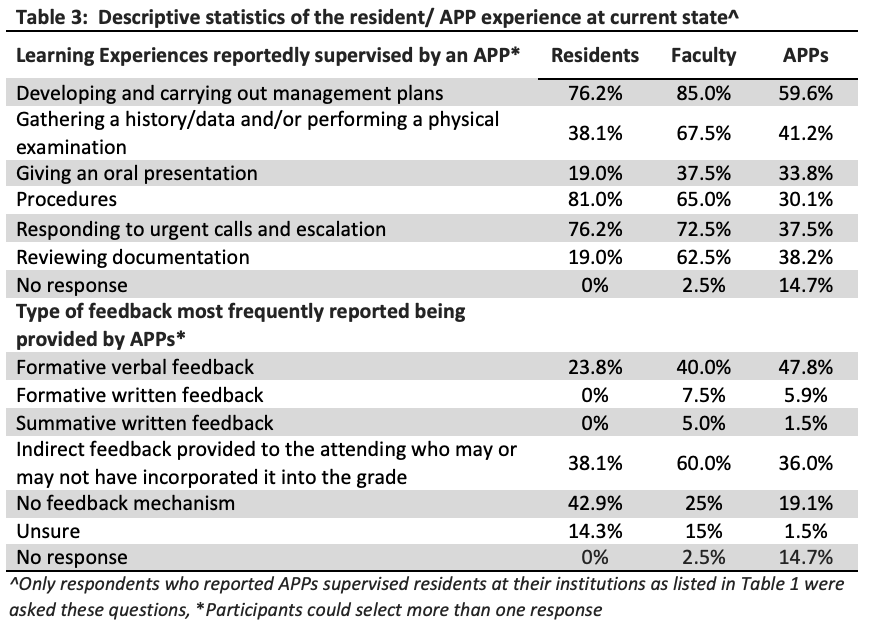
Table 4: Comparison of Stakeholder Perceptions of the APP Role in MS Education; Table 5: Comparison of Stakeholder Perceptions of the APP Role in Resident Education