Children with Chronic Conditions 4
Session: Children with Chronic Conditions 4
482 - Respite and Personal Care Services for Children with Medical Complexity: A Thematic Analysis of One State's Complex System
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 482.6256
Makenzie B. Morgen, UW-Health, Madison, WI, United States; Sanaa Semia, University of Wisconsin School of Medicine and Public Health, Cottage Grove, WI, United States; Abby Hammes, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States; Mary L. Ehlenbach, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States

Makenzie B. Morgen, BA (she/her/hers)
Medical Student
University of Wisconsin Madison School of Medicine and Public Health
Madison, Wisconsin, United States
Presenting Author(s)
Background: Children with Medical Complexity (CMC) have unique needs that extend to their homes and communities. CMC frequently have challenges accessing the support and services for which they are eligible, including personal care (PC) and respite services. Further understanding of barriers and facilitators to achieving adequate PC and respite services for CMC is critical to efficiently improving access to these essential home- and community-based services systems that support health equity for CMC and their families.
Objective: This project aims to describe barriers and facilitators to accessing personal care and respite services for CMC living at home in Wisconsin.
Design/Methods: From June to August 2024, thirteen semi-structured conversations using qualitative interview techniques were conducted. Seven focus groups of lived-experience experts in a variety of disciplines, including parents of CMC (n=9), private duty nurses (n=6), personal care and/or respite providers (n=5), and children’s hospital-based healthcare professionals (n=5) were performed. Six key informant interviews with family advocacy experts and healthcare professionals with expertise in authorization and/or delivery of home- and community-based services throughout the state were completed. All conversations were conducted virtually, recorded, transcribed, and dual-coded. Codes were analyzed iteratively to identify shared concepts and generate emergent themes describing barriers and facilitators to PC and respite services for CMC.
Results: Five themes emerged from the thematic analysis. First, PC and respite services are essential to the health and well-being of CMC and their families. Second, the current structure of the service authorization and delivery system is not patient-centered, making it a barrier to accessing services. Third, provision of PC and respite services is not valued as a career, thereby limiting recruitment and retention of qualified workers. Fourth, obtaining PC and respite services for a CMC involves a large family workload and investment. Finally, solutions and facilitators of system improvement were identified by participants (Table 1).
Conclusion(s): Families of CMC face many barriers to achieving adequate PC and respite care for their child with disabilities. Future directions should focus on further understanding the root causes of identified barriers and implementing targeted interventions to address these causes, with focus on the solutions suggested by lived-experience experts.
Table 1.
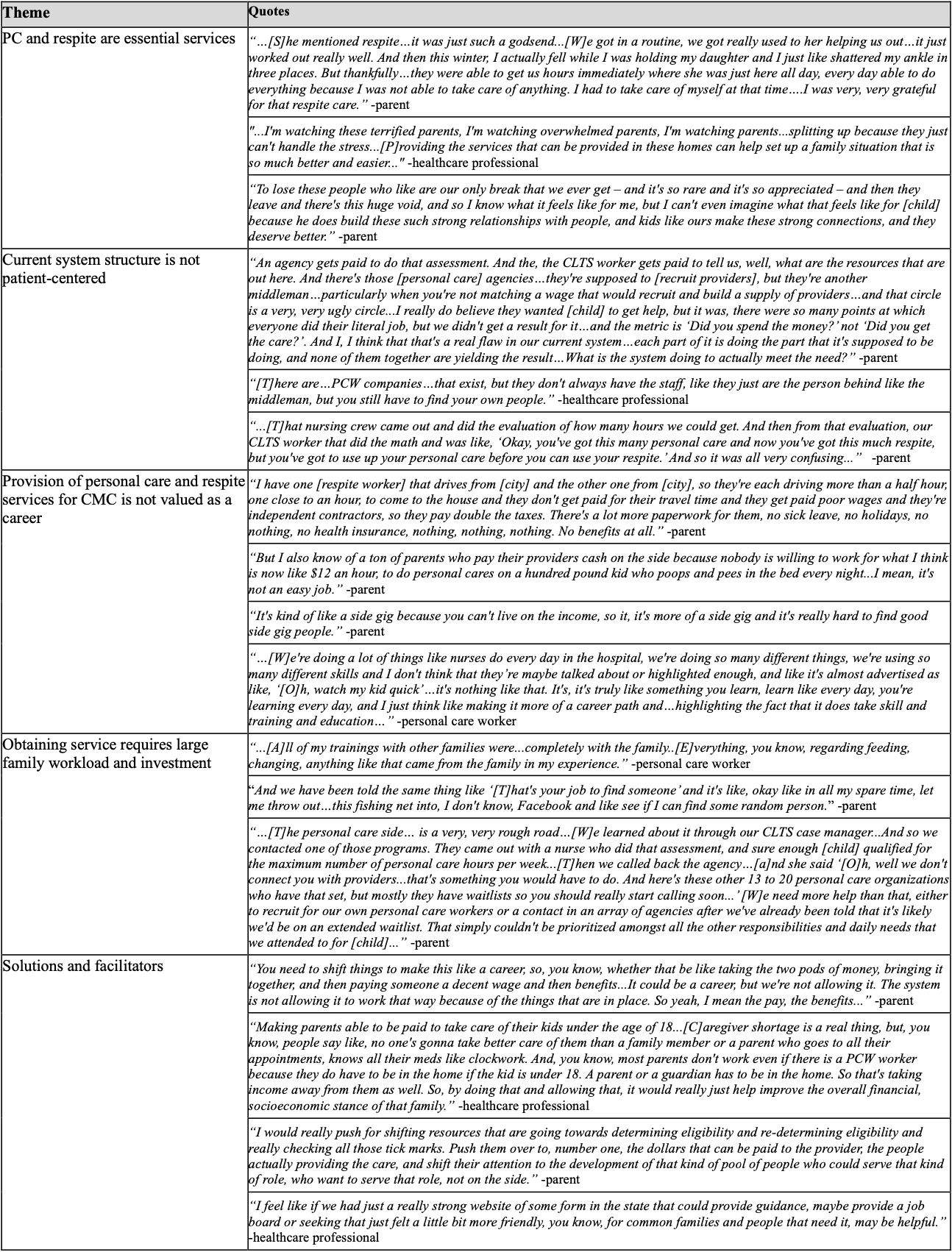 Quotes from focus groups and key informant interviews highlighting the identified themes
Quotes from focus groups and key informant interviews highlighting the identified themes
