Mental Health 4
Session: Mental Health 4
099 - Hospital-Level Factors Associated with Length of Stay for Children Hospitalized Due to Suicide Attempt or Self-Injury Among US Children’s Hospitals
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 99.5195
Cory Alexieff, K. Hovnanian Children's Hospital at Jersey Shore University Medical Center, Red Bank, NJ, United States; Adrienne DePorre, Children's Mercy Hospitals and Clinics, Kansas City, MO, United States; Matthew Hall, Children's Hospital Association, Lenexa, KS, United States; Daniel A. Rauch, Hackensack Meridian School of Medicine, Hackensack, NJ, United States; Jay Berry, Complex Care, Boston Children's Hospital, Boston, MA, United States; Yen-Hong Kuo, Hackensack Meridian School of Medicine, Neptune, NJ, United States; Jamie M. Pinto, K. Hovnanian Children's Hospital at Jersey Shore University Medical Center, Neptune, NJ, United States
- CA
Cory Alexieff, DO (he/him/his)
Pediatric Hospital Medicine Fellow
K. Hovnanian Children's Hospital at Jersey Shore University Medical Center
Red Bank, New Jersey, United States
Presenting Author(s)
Background: Suicide attempt and self-injury (SA/SI) are frequent reasons for medical hospitalizations, yet little is known about length of stay (LOS) among youth hospitalized for SA/SI. LOS is commonly used to measure quality of patient care and resource use within hospitals, and a comprehensive understanding of factors associated with LOS among youth admitted for SA/SI is particularly critical, as hospitals often lack the mental health resources needed to care for patients with SA/SI. Among patients with SA/SI, shorter LOS may expedite access to dedicated mental health treatment and promote optimization of hospital resources.
Objective: To describe variation in hospital LOS among children admitted with SA/SI, and explore hospital factors associated with LOS
Design/Methods: We studied hospitalizations of children aged 5-18 years with a primary diagnosis of SA/SI from 2022-2023 across 43 US children’s hospitals using the Pediatric Health Information System database. Each hospital's mean LOS was adjusted using age, sex, race, payor, and illness severity. A hospital was categorized as an outlier if the 95% CI for its adjusted mean did not include the grand mean. Hospital factors hypothesized to affect LOS in this population were identified using the Children’s Hospital Association Annual Benchmark Report. Generalized Estimating Equations were used to determine hospital factors associated with LOS clustering on hospitals.
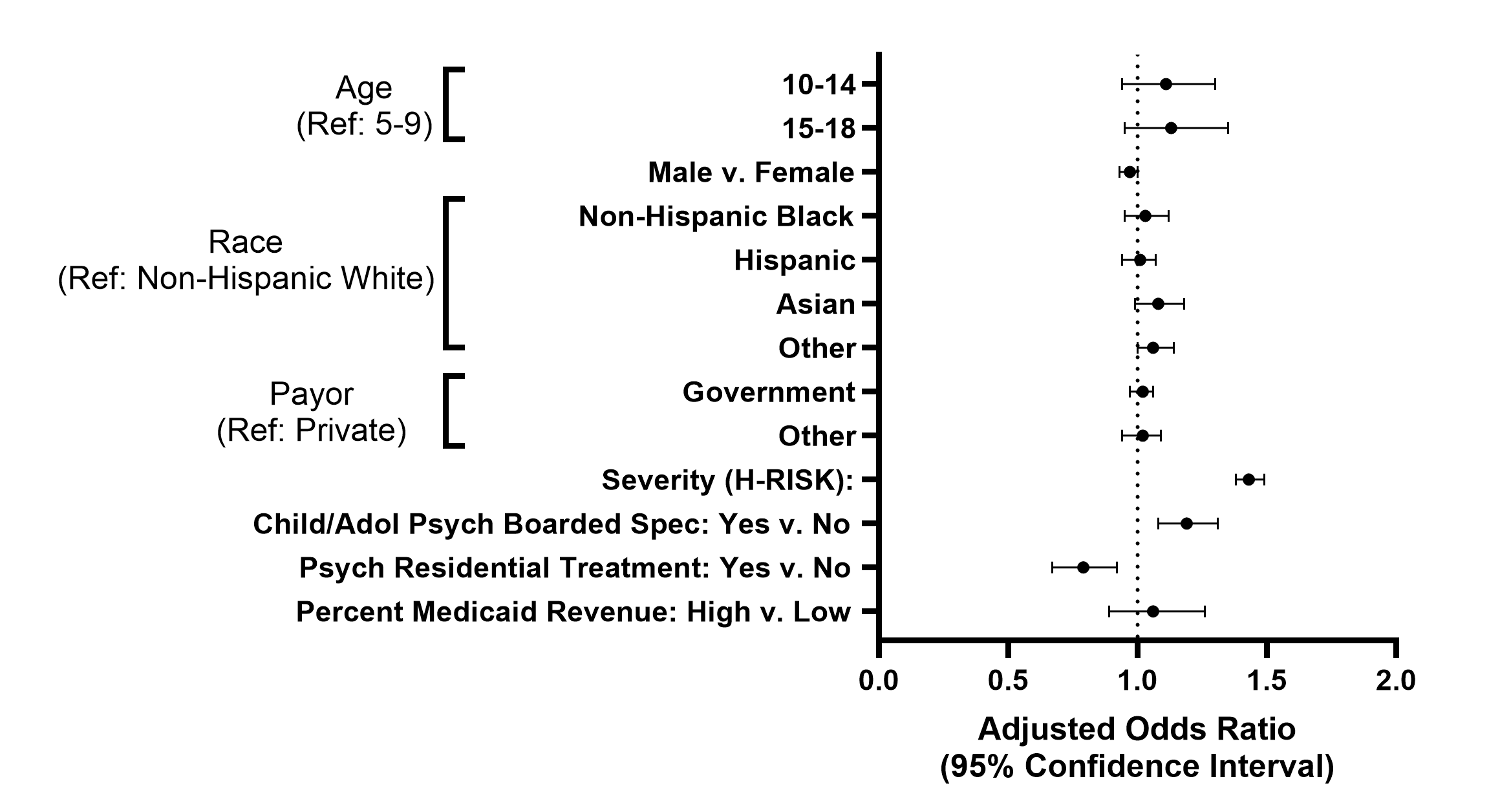
Results: We identified 19,196 hospitalizations, with mean LOS of 2.10 [IQR 1.24-5.15] days. Adjusted analysis showed wide variation in LOS across hospitals (Figure 1). Adjusted univariate analysis demonstrated significant association of shorter LOS with the presence of an inpatient psychiatric residential treatment program. Conversely, the presence of Child and Adolescent Psychiatry boarded specialists and low % Medicaid revenue were both associated with longer LOS (Table 1). In multivariable modeling, shorter LOS remained significantly associated with psychiatric residential treatment programs and longer LOS remained significantly associated with the presence of Child and Adolescent Psychiatry boarded specialists (Figure 2).
Conclusion(s): We found substantial variation in adjusted mean LOS among children hospitalized for SA/SI. Hospital factors significantly associated with LOS included presence of psychiatry specialists and inpatient psychiatric residential treatment programs. These findings can inform children’s hospitals in prioritizing interventions that reduce LOS in acute care settings, which could facilitate faster transitions to acute psychiatric care and optimize use of hospital resources.
Figure 1. Adjusted mean LOS by hospital for hospitalizations with primary diagnosis of SA/SI
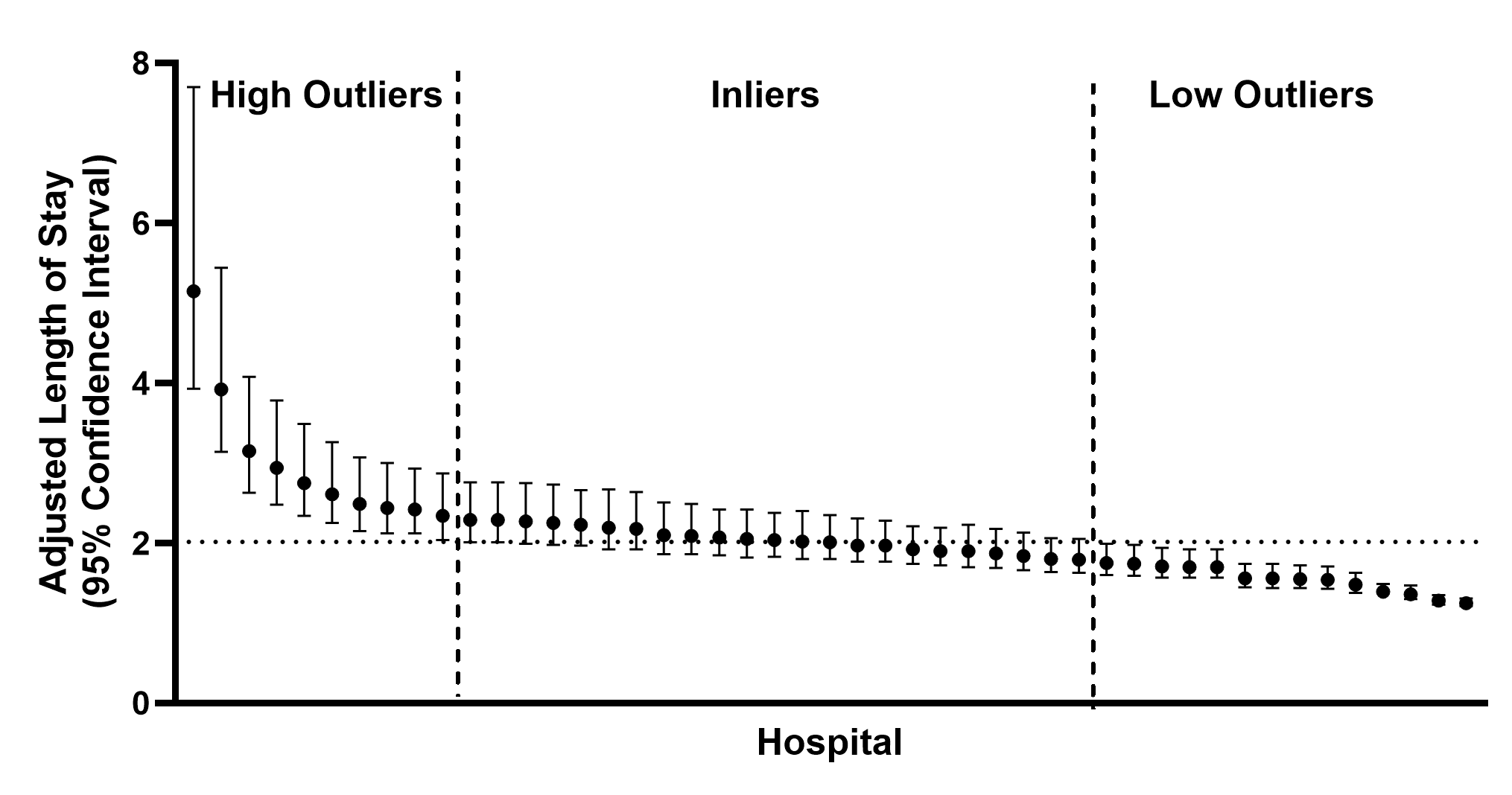 Length of Stay measured in days. Each data point represents a unique PHIS-reporting hospital. Horizontal dotted line represents grand mean across all hospitals.
Length of Stay measured in days. Each data point represents a unique PHIS-reporting hospital. Horizontal dotted line represents grand mean across all hospitals.Table 1. Adjusted mean LOS for SA/SI hospitalizations by hospital factor
.png) Length of Stay measured in days. Qualitative factors were dichotomized for the presence or absence of each item. Quantitative factors were dichotomized into “high” and “low” categories based on their relation to the median value amongst all hospitals. For example, median Medicaid Revenue was 54.2% and values above this were counted as “High Percent Medicaid Revenue”. FTE: full-time equivalent. AOM: adjusted occupied bed.
Length of Stay measured in days. Qualitative factors were dichotomized for the presence or absence of each item. Quantitative factors were dichotomized into “high” and “low” categories based on their relation to the median value amongst all hospitals. For example, median Medicaid Revenue was 54.2% and values above this were counted as “High Percent Medicaid Revenue”. FTE: full-time equivalent. AOM: adjusted occupied bed.Figure 2. Multivariable model of factors associated with LOS for SA/SI hospitalizations
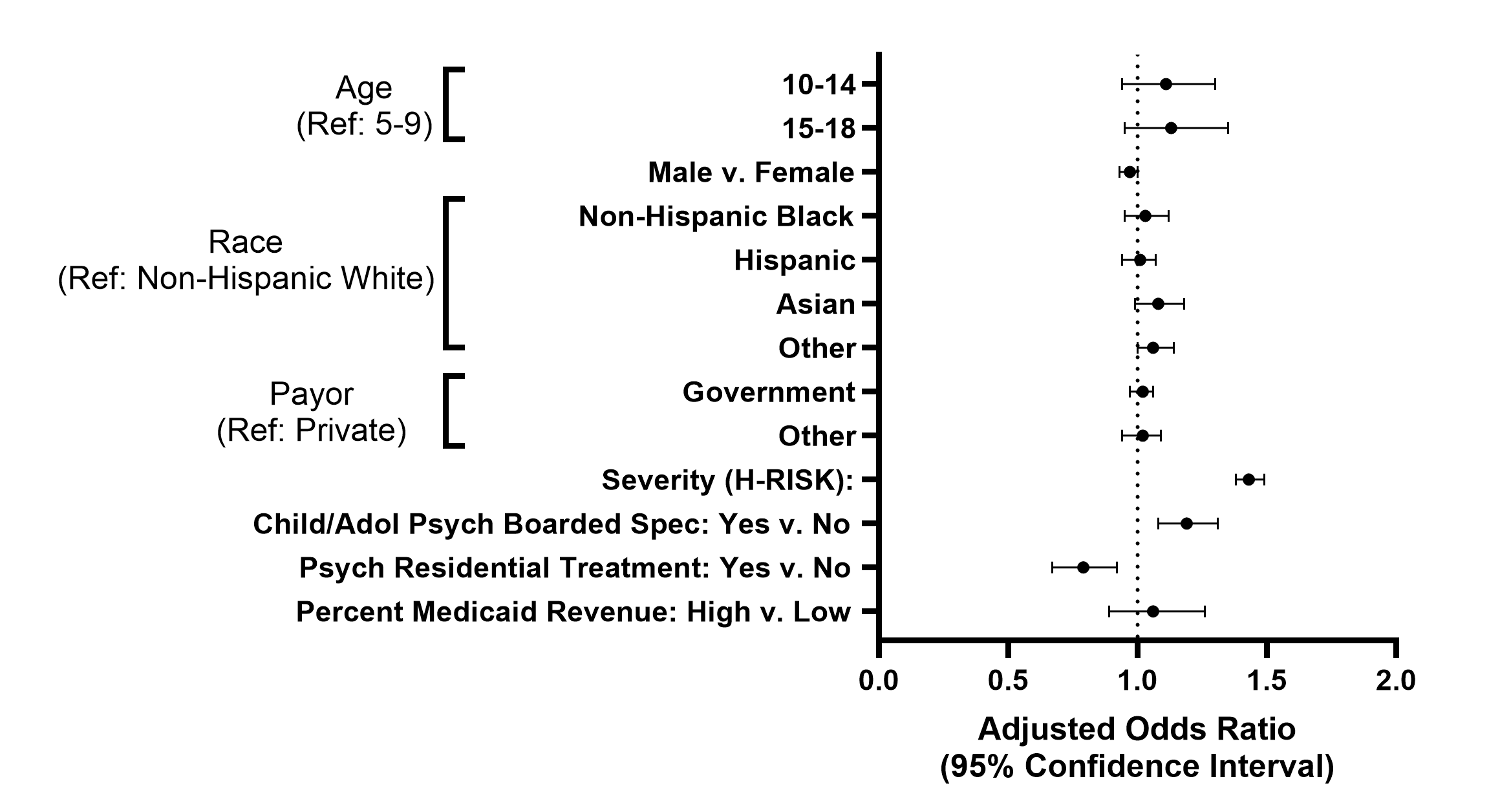
Figure 1. Adjusted mean LOS by hospital for hospitalizations with primary diagnosis of SA/SI
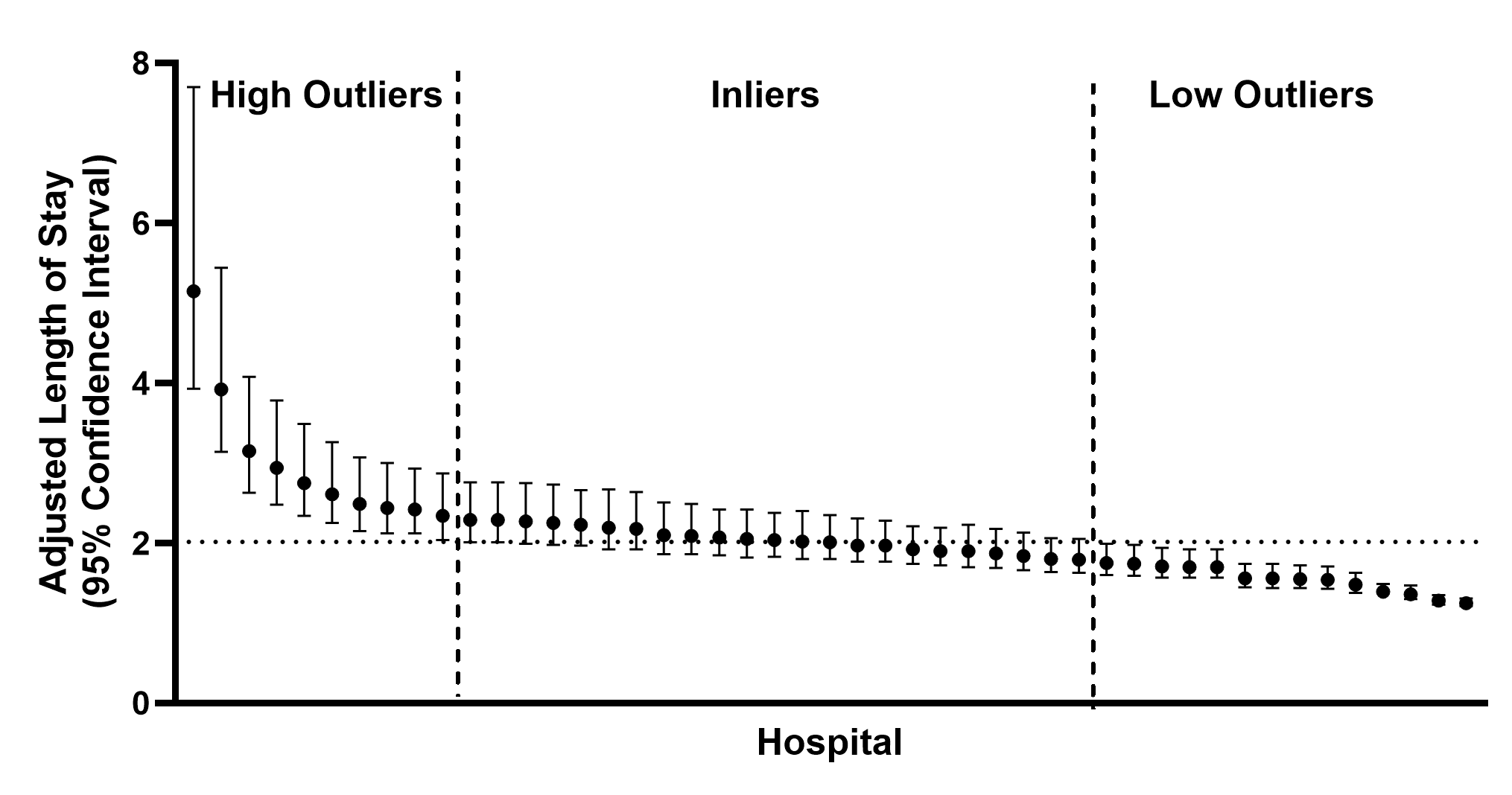 Length of Stay measured in days. Each data point represents a unique PHIS-reporting hospital. Horizontal dotted line represents grand mean across all hospitals.
Length of Stay measured in days. Each data point represents a unique PHIS-reporting hospital. Horizontal dotted line represents grand mean across all hospitals.Table 1. Adjusted mean LOS for SA/SI hospitalizations by hospital factor
.png) Length of Stay measured in days. Qualitative factors were dichotomized for the presence or absence of each item. Quantitative factors were dichotomized into “high” and “low” categories based on their relation to the median value amongst all hospitals. For example, median Medicaid Revenue was 54.2% and values above this were counted as “High Percent Medicaid Revenue”. FTE: full-time equivalent. AOM: adjusted occupied bed.
Length of Stay measured in days. Qualitative factors were dichotomized for the presence or absence of each item. Quantitative factors were dichotomized into “high” and “low” categories based on their relation to the median value amongst all hospitals. For example, median Medicaid Revenue was 54.2% and values above this were counted as “High Percent Medicaid Revenue”. FTE: full-time equivalent. AOM: adjusted occupied bed.Figure 2. Multivariable model of factors associated with LOS for SA/SI hospitalizations