Critical Care 4
Session: Critical Care 4
501 - Functional Status Outcomes in Pediatric ECMO Survivors
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 501.4900
Sarah L. Greenfield, University of Texas Southwestern Medical School, Dallas, TX, United States; Ishaan Sangwan, UCSF, San Francisco, CA, United States; Michael C. Morriss, University of Texas Southwestern Medical School, Flower Mound, TX, United States; Sumit Singh, UT Southwestern Medical Center, Dallas, TX, United States; Xilong Li, UT Southwestern Medical Center, Dallas, TX, United States; Laura Hatton, Children's Health, Fort Worth, TX, United States; Margarita Ramos, Children's Health, Garland, TX, United States; Ricardo Medrano, Children's Health, Dallas, TX, United States; Lakshmi Raman, University of Texas Southwestern Medical Center, Dallas, TX, United States; Erin L. Tresselt, University of Texas Southwestern Medical School, Dallas, TX, United States

Sarah L. Greenfield, MD (she/her/hers)
Resident Physician
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Pediatric extracorporeal membrane oxygenation (ECMO) utilization is rising. ECMO survivors are at risk for adverse neurodevelopmental effects due to illness severity and complications of ECMO. Up to 50% of ECMO survivors experience delay or disability and many suffer school and behavioral difficulties and memory and attention deficits. ELSO recommends follow-up to address deficits that can be missed by standard developmental screening measures, however no standardized tools are recommended. Post-ECMO neuroimaging is often performed but has not been correlated with functional outcomes.
Objective: To investigate neurodevelopmental outcomes of ECMO survivors using Adaptive Behavioral Assessment System (ABAS) and Functional Status score (FSS) which will be followed by comparison to neuroimaging severity scoring.
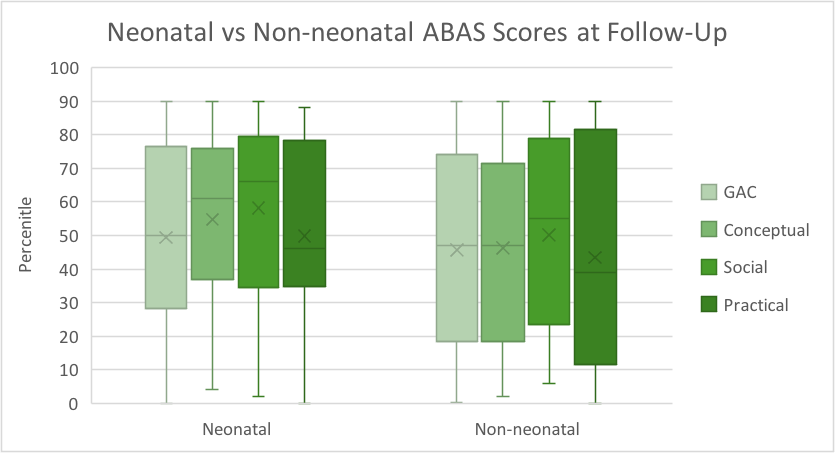
Design/Methods: Children aged 0-18 cannulated to ECMO between 2020 and 2024 at our single center who survived to follow-up period were included. ABAS evaluates skills in Global Adaptive Composite (GAC), Conceptual, Social and Practical domains. For patients ≥ 60 days old, caregivers completed ABAS within 72 hours of cannulation. A repeat survey was administered 6-18 months after decannulation. FSS was noted at time of discharge and follow-up.
Post-ECMO neuroimaging will be scored as mild, moderate, or severe by an independent and blinded neuroradiologist following established precedent. Scores will be compared to ABAS-3 and FSS results.
Results: 42 patients completed follow-up screening. Average age at cannulation was 34 months and 40% of patients were neonates. 15 patients (36%) were cannulated to VV ECMO. Of VA cases, 10 (23%) were cannulated centrally. Average pre-cannulation vasoactive inotropic score (VIS) was 18.8 for VA and 10.6 for VV patients.
Practical scores were lowest for both neonatal (median 46, IQR 40) and non-neonatal patients (median 39, IQR 68). Median GAC at follow up in non-neonates was 47th percentile (IQR 52) vs 50th in neonates (IQR 42).
FSS at follow up was higher in the VA group (mean 7.8, 69% ≥7) vs the VV group (mean 6.1, 7% ≥7) with chi square 14.2, p 0.014.
Conclusion(s): Pediatric VA ECMO survivors are more likely to experience functional impairment and medical equipment dependence compared to VV ECMO patients. Though median ABAS scoring is near average for age, there is wide variation and correlation with pre-cannulation scores is needed. Neuroimaging scores may help prognosticate function for families of ECMO survivors.
Neonatal vs Non-Neonatal ABAS Scores at Follow-Up