Neonatal Pulmonology - Basic/Translational Science 3
Session: Neonatal Pulmonology - Basic/Translational Science 3
317 - Evaluating the Accuracy of an Online Bronchopulmonary Dysplasia Risk Estimator: A Multicenter Study
Monday, April 28, 2025
7:00am - 9:15am HST
Publication Number: 317.4899
Ana H. Martinez, Johns Hopkins All Children's Hospital, St. Petersburg, FL, United States; John Morrison, Johns Hopkins All Children's Hospital, Saint Petersburg, FL, United States; Joseph Manipadam, Johns Hopkins All Children's Hospital, Tampa, FL, United States; Jamie L. Fierstein, Johns Hopkins All Children's Hospital, St. Petersburg, FL, United States; Vera Ignjatovic, Johns Hopkins All Children's Hospital Institute for Clinical and Translational Research, St. Petersburg, FL, United States; Joana Machry, MD, Johns Hopkins All Children's Hospital Institute for Clinical and Translational Research, St. Petersburg, FL, United States
.jpg)
Ana H. Martinez, MD (she/her/hers)
Fellow
Johns Hopkins All Children's Hospital
St. Petersburg, Florida, United States
Presenting Author(s)
Background: Identifying neonates at highest risk of bronchopulmonary dysplasia (BPD) is important to guide therapeutic interventions that are potentially disease course altering. Postnatal corticosteroids (PNC) prescribed for predicted BPD/mortality risk >60% (2011 NICHD BPD risk estimator) has been our evidence-based approach. However, the updated 2022 NICHD risk estimator resulted in fewer neonates meeting PNC eligibility criteria, prompting need to evaluate the accuracy of the 2022 estimator in predicting risk for combined BPD/mortality in our population and validation of optimal cutoff to indicate PNC therapy.
Objective: Assess the predictive accuracy of the 2022 NICHD BPD risk estimator in identifying neonates at risk for BPD Grade 2/3 and/or death for the population of neonates at three Johns Hopkins Health System NICUs.
Design/Methods: Retrospective cohort study of infants < 28 weeks gestation admitted before 28 days of life (DOL) to Johns Hopkins NICUs between January 2022 and September 2024. The primary predictor was the 2022 NICHD BPD outcome estimator risk score, and the primary outcome was BPD grade 2/3 and/or death. Exclusion criteria: death prior to 28 DOL, missing data for 2022 NCHD BPD risk estimation. Data was extracted from the medical records of each institution as part of a larger BPD Quality Improvement Initiative. Demographic and clinical data were summarized. Accuracy of the risk calculator and an optimized cutoff for consideration of PNC administration was assessed using area under the receiver operating characteristic curve (ROC) analyses.
Results: Neonates meeting inclusion criteria and surviving to time of diagnosis of BPD were 212/214. Neonates with the outcome of grade 2/3 BPD or death had significantly lower BW and GA at birth (p < 0.001), were more likely to be male gender (p < 0.004), have a higher estimated risk (p=0.002) and to receive multiple courses of PNC (p < 0.03) (Table 1). The 2022 BPD estimator was a good predictor for BPD and death (AUC = 0.83, 95% confidence interval 0.75-0.86, Fig. 1). Around 34% of the patients developing grade 2/3 BPD or death had a risk estimation between 40% and 60% and around 36% had a risk estimation of less than 40% (Fig. 2).
Conclusion(s): The 2022 BPD risk estimator was accurate at predicting the outcome of BPD and death, however at this time an optimal cut off for treatment with PNC could not be determined. Most of the patients who had the outcome of grade 2/3 BPD or Death had a risk estimation that was below the currently agree on cut-off of 60%. Further research is necessary to clarify a new cut-off.
Table 1
.png) Demographic and outcomes comparing neonates who had a diagnosis of grade 2/3 BPD and those who had no BPD (grade 0) or grade 1 BPD. GA: gestational age; BW: birth weight; SC: systemic corticosteroids; cGA: corrected gestational age; DOL: day of life.
Demographic and outcomes comparing neonates who had a diagnosis of grade 2/3 BPD and those who had no BPD (grade 0) or grade 1 BPD. GA: gestational age; BW: birth weight; SC: systemic corticosteroids; cGA: corrected gestational age; DOL: day of life.Figure 1
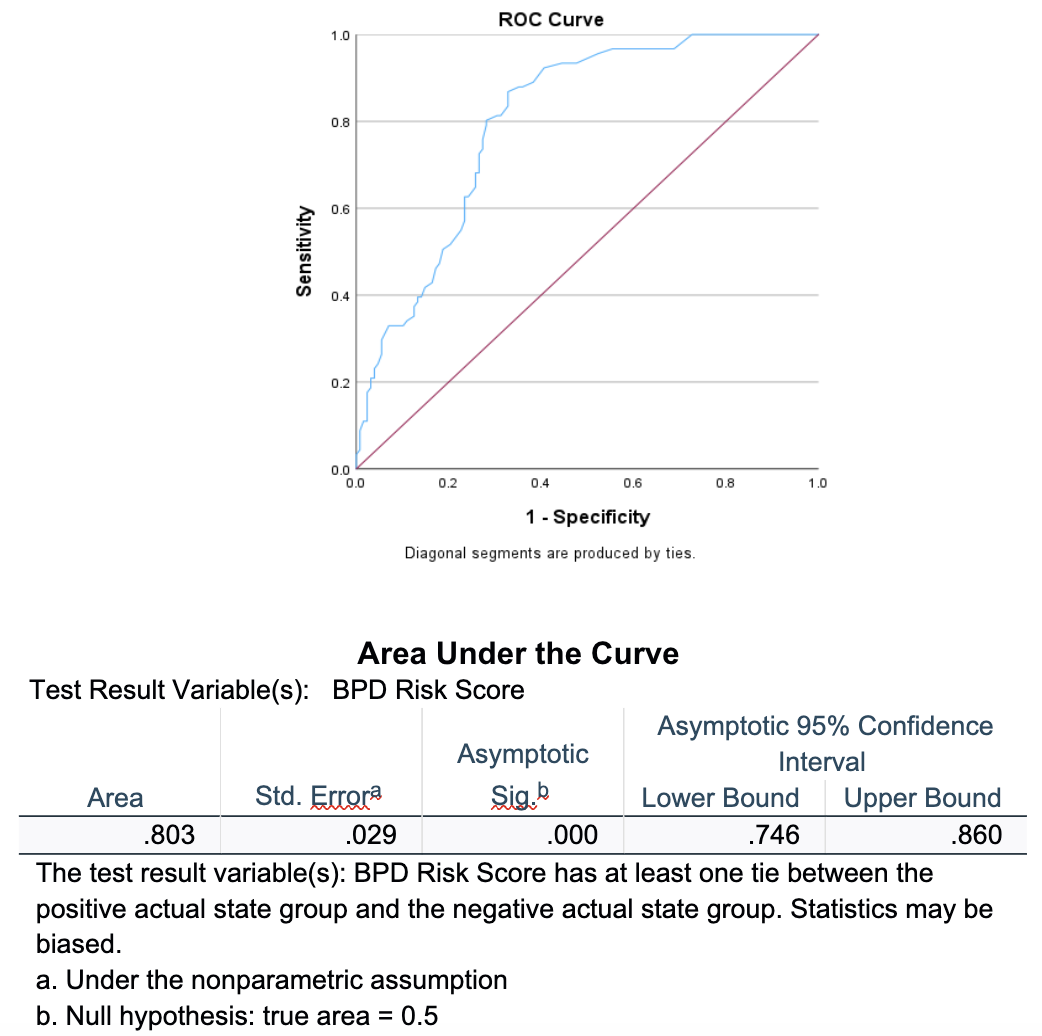 ROC curve showing NICHD BPD risk estimation of grade 2 and 3 BPD and death as a predictor of actual development of the disease.
ROC curve showing NICHD BPD risk estimation of grade 2 and 3 BPD and death as a predictor of actual development of the disease.Figure 2
.png) Boxplots of both groups 0= BPD grade 0/1 and 1= BPD grade 2/3/ Death. Around 73% of the patients in group 0 fall under 40% risk and around 36% of group 1 patients fall under the 40% cut off, however most of group 1 patients fall under 60% (around 66%).
Boxplots of both groups 0= BPD grade 0/1 and 1= BPD grade 2/3/ Death. Around 73% of the patients in group 0 fall under 40% risk and around 36% of group 1 patients fall under the 40% cut off, however most of group 1 patients fall under 60% (around 66%). 
