Emergency Medicine 1
Session: Emergency Medicine 1
418 - Process Simulation for Design of New Emergency Department Workflows
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 418.6252
Jean I. Pearce, Medical College of Wisconsin, Milwaukee, WI, United States; Sarah E.. Thill, Medical College of Wisconsin, Milwaukee, WI, United States; Abigail Schuh, Medical College of Wisconsin, Menomonee Falls, WI, United States; Viday Heffner, Medical College of Wisconsin, Wauwatosa, WI, United States; Meagan Ladell, Medical College of Wisconsin, Milw, WI, United States; Madeline E. Winn, Medical College of Wisconsin, Milwaukee, WI, United States; Mariah Marino, Children's Hospital of Wisconsin, Milwaukee, WI, United States; Amy L.. Drendel, Medical College of Wisconsin, Milwaukee, WI, United States
- JP
Jean I. Pearce, MD, M.S. (she/her/hers)
Associate Professor of Pediatrics
Medical College of Wisconsin
Milwaukee, Wisconsin, United States
Presenting Author(s)
Background: A new emergency department (ED) was built with a different footprint and increased patient beds but unchanged staff numbers. With ongoing care and the inability to control patient arrivals, optimizing efficiency prior to transition was necessary. Historically, process simulation has been used to identify latencies in hospital flow and design. No study has evaluated the efficacy of process simulation on patient flow metrics in a new ED.
Objective: Utilize process simulation to evaluate, test, and refine ED workflows and measure patient flow impact using time-bound metrics one week pre- and post-ED opening.
Design/Methods: Content experts identified key ED workflows impacted by the new environment to develop twelve process simulation scenarios. Two-hour process simulation sessions using a high-fidelity mannequin were conducted over eight weeks with key multidisciplinary stakeholders in the new physical space with mock-ups of equipment/supplies to evaluate, test and adapt ED workflow changes. After each simulation, a trained simulation facilitator conducted a debrief focusing on latencies and changes recommended to inform the final workflows that were implemented. Standard patient flow metrics including arrival to room, arrival to provider, provider to disposition, disposition to discharge/admission, and length of stay for discharged and admitted patients were collected 1 week pre- and post-ED opening. Descriptive statistics and Wilcoxon signed rank tests were calculated.
Results: There were 33 participants in the process simulations from 9 disciplines (Table 1). Rich feedback collected during the debrief identified themes around equipment location/physical space, communication, medication acquisition, personnel/teams, workflows, pathways, and staff education that were utilized to develop and refine workflows that were implemented prior to ED opening (Table 2). Pre- and post-opening, there was a significant difference in ED daily patient volumes (183 vs 205, p = 0.03) and arrival to room times (10 vs 4 minutes, p = 0.02). Other patient flow metrics were unchanged including arrival to provider, arrival to disposition, disposition to discharge/admit, and length of stay for discharges and admissions (Table 3).
Conclusion(s): This novel application of process simulation resulted in improved or sustained patient flow metrics immediately following the transition to a new ED despite working in a larger space with the same number of staff and more patients. Identification of latencies with space, equipment, and ED processes resulted in improved workflow implementation.
Table 1
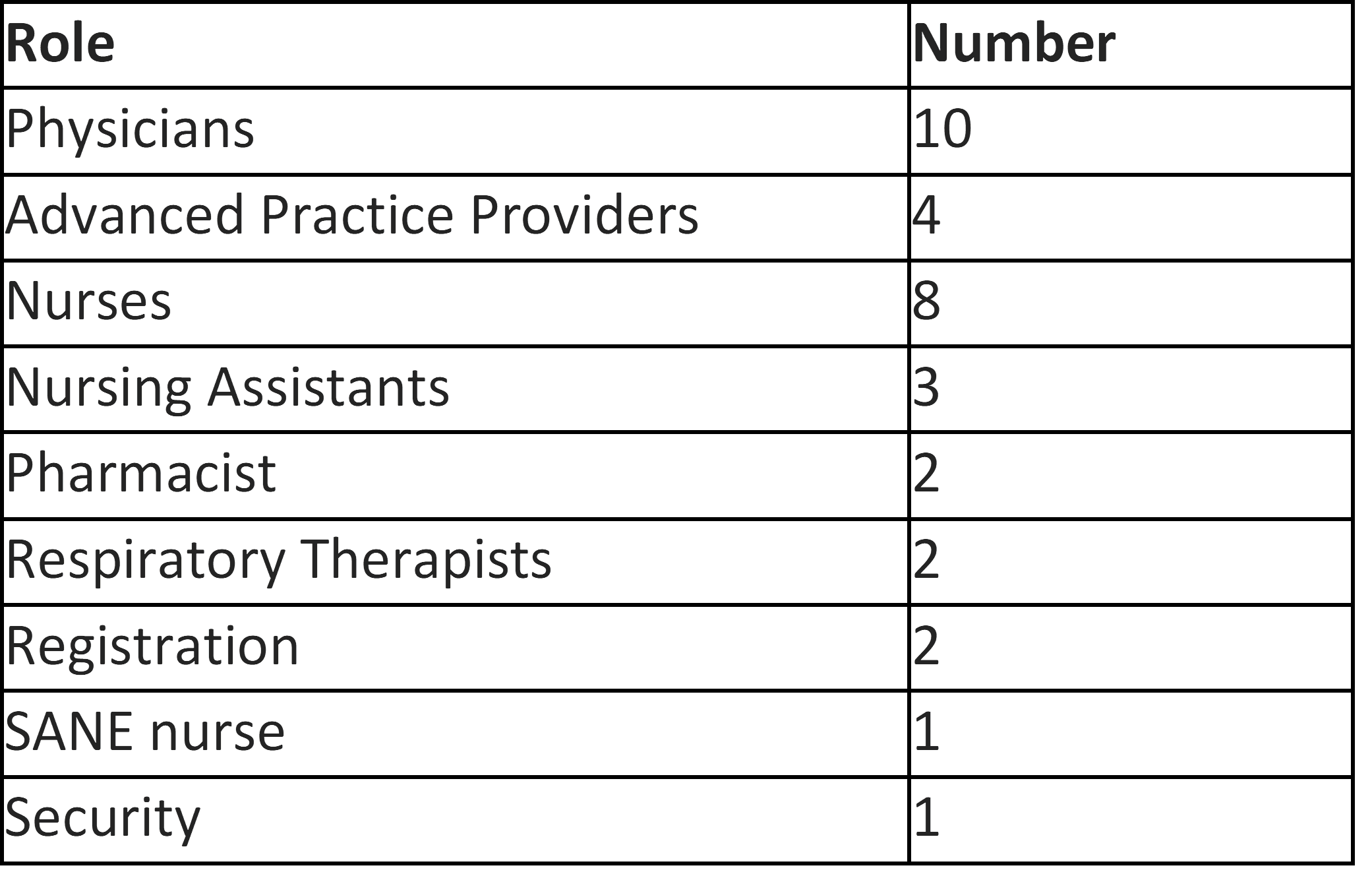 Number of participants in each discipline.
Number of participants in each discipline.Table 2
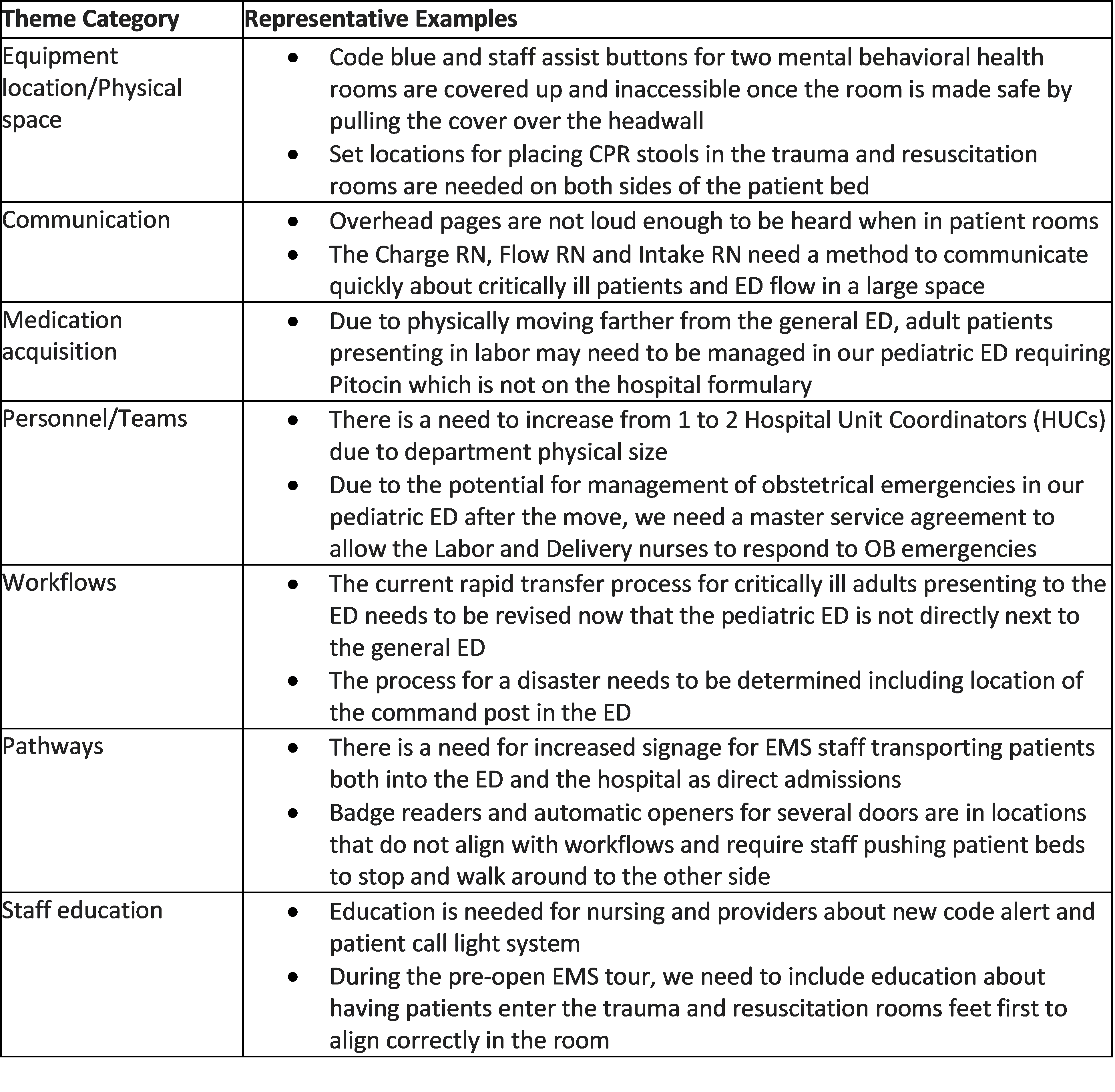 Content themes with representative examples identified during process simulations.
Content themes with representative examples identified during process simulations.Table 3
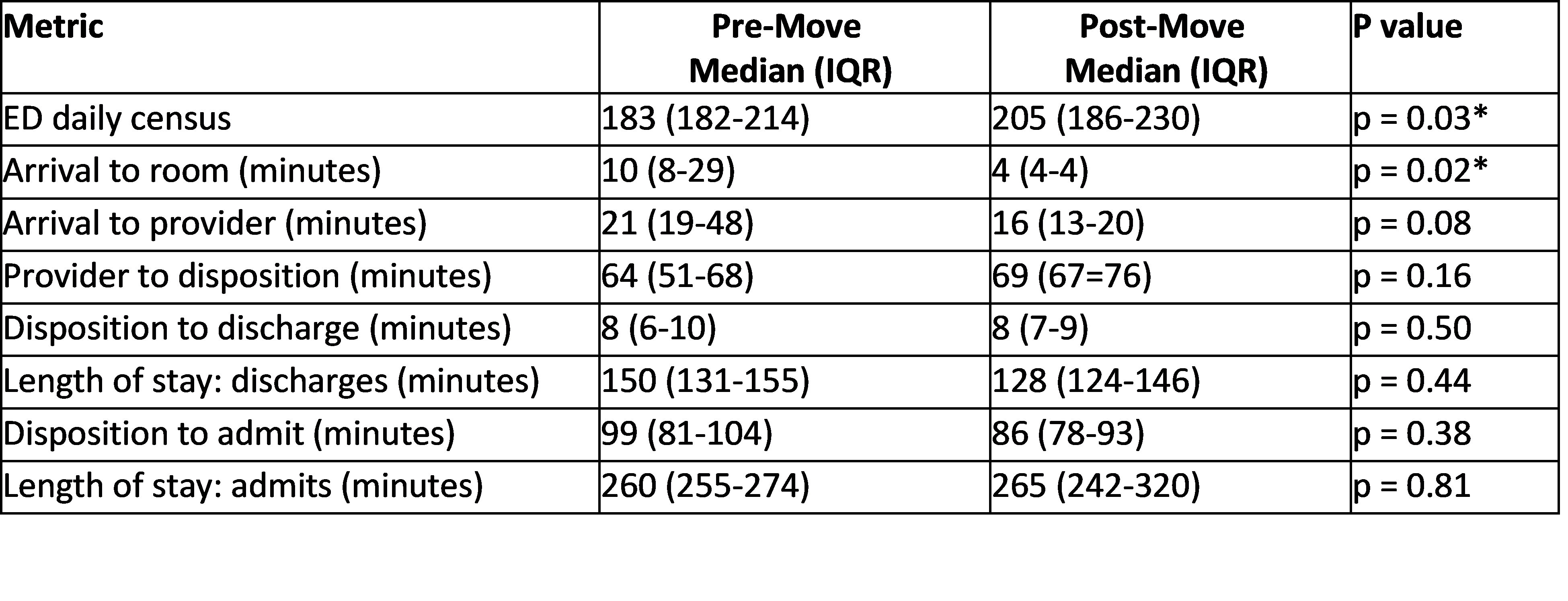 Pre- and post-ED move patient flow metrics.
Pre- and post-ED move patient flow metrics.
