Critical Care 2
Session: Critical Care 2
120 - Ability of pSOFA at 48 hours to Predict Mortality in Pediatric Patients with Severe Traumatic Brain Injury
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 120.3781
Jefferson Bedell, UTMB, Houston, TX, United States; Syed S.. Hashmi, McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, TX, United States; Thao L. Nguyen, McGovern Medical School at the University of Texas Health Science Center at Houston, Houston, TX, United States; Chinyere O’Connor, UTHealth Houston, Houston, TX, United States
- JB
Jefferson Bedell, II, MD (he/him/his)
Associate Professor
UTMB
Houston, Texas, United States
Presenting Author(s)
Background: Traumatic brain injuries (TBIs) are major contributors to death and disability in the pediatric population. Prognostic predictors in severe pediatric TBI are not well explored.
Objective: We aim to investigate differences in the characteristics of prognostic predictors among pediatric patients with severe TBI patients, with the primary outcome of mortality.
Design/Methods: This was a retrospective descriptive study over 10 years (2012-2022). We compared prognostic scores against the primary outcome of mortality over the first 72hours of admission to the critical care unit. Prognostic scores applied were the Pediatric Risk of Mortality (PRSIM) III at 24hrs and the daily pediatric Sequential Organ Failure Assessment score (pSOFA) for each of the 3 days from admission. Fisher exact test and Mann-Whitney U test were conducted, along with an assessment of predictive ability of the scores using the receiver operating characteristic curve.
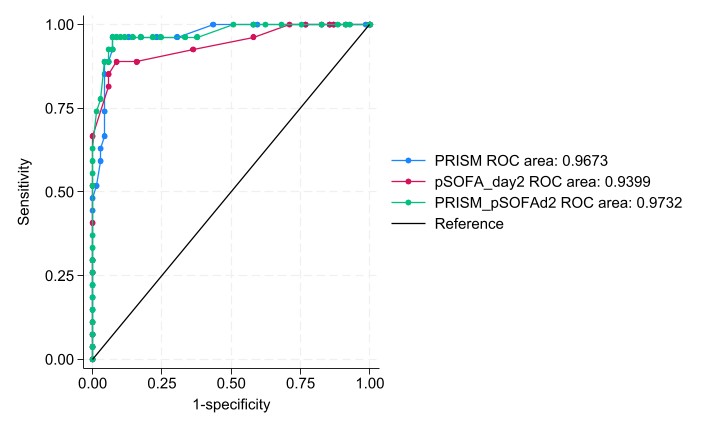
Results: A total of 97 patients with TBI were identified. There was a greater improvement in pS0FA-day2 (d2) and day3 scores (i.e. a negative change in scores) post-admission (p < 0.001 and p=0.008, respectively) among patients that got discharged compared to those that died (Table 1). PRISM III and pSOFA-d2 provided independent prognostication, suggesting that together they may be able to provide improved prognostication of mortality past 48 hours if used in combination. To assess this ability of PRISM III and pSOFA-d2 in combination, a new scoring tool was created that summed up the scores from PRISM III and p-SOFA-d2 (PRISM-pSOFAd2). PRISM-pSOFAd2 had a slightly higher Area Under the Curve (AUC) (0.973) and pSOFA-d2 had a slightly lower AUC (0.940) compared to PRISM III (AUC=0.967) but these differences in predictive ability between PRISM III and pSOFA-d2 or the combined PRISM-pSOFAd2 were not statistically significant (Table 2; Fig 1).
Conclusion(s): Outcome prediction is crucial for guiding goals of care conversation with families and in standardizing research across institutions. The PRISM III score is useful only in the first 24 hours and is challenging to measure at the bedside. pSOFA-d2 can provide a means to predict mortality that is comparable to the predictive ability of PRISM III at admission. This can be helpful in scenarios where the PRISM III was not calculated at admission or early during the first day, especially in situations where lack of resources limits the ability to calculate the PRISM III score.
Table 1: Comparison of prognostic scores between patients that died and those discharged at 72 hours post-admission
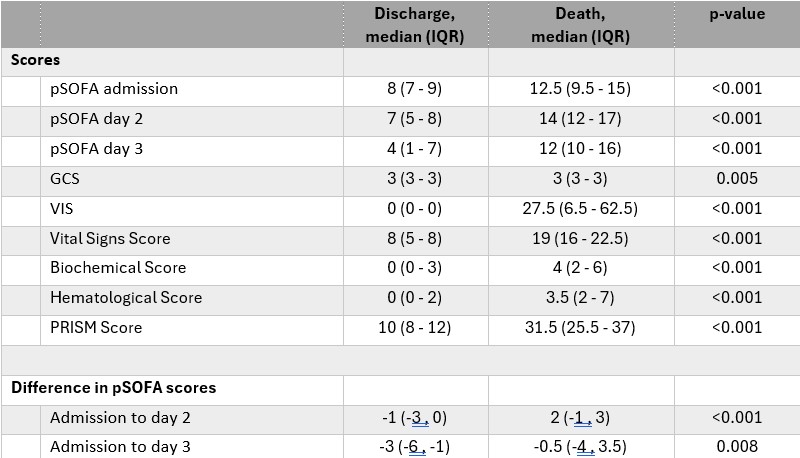 pediatric Sequential Organ Failure Assessment score (pSOFA); GCS, glascow coma scale; VIS, vaso-inotropic support; Pediatric Risk of Mortality (PRSIM) III at 24hrs
pediatric Sequential Organ Failure Assessment score (pSOFA); GCS, glascow coma scale; VIS, vaso-inotropic support; Pediatric Risk of Mortality (PRSIM) III at 24hrs Table 2. Area under the curve (AUC) and 95% confidence intervals for various prognostic models to assess their ability to predict mortality
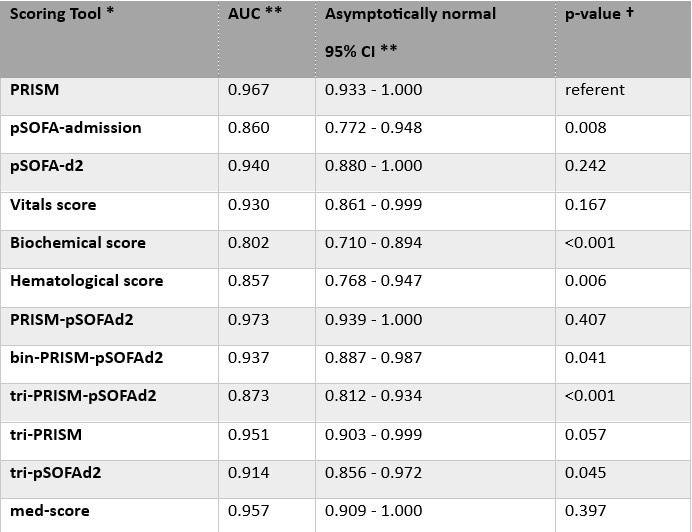 * Description of each of the scores is listed in the body of the results document
* Description of each of the scores is listed in the body of the results document** AUC = area under the curve from ROC analysis; 95% CI = 95% confidence interval
† p-value from comparison of AUC of each score and the PRISM score
pediatric Sequential Organ Failure Assessment score (pSOFA); Pediatric Risk of Mortality (PRSIM) III at 24hrs.
The scores assessed included PRISM, pSOFA-admission, pSOFA-d2, Vitals score, Biochemical score, Hematological score, PRISM-pSOFAd2, bin-PRISM-pSOFAd2, tri-PRISM-pSOFAd2, and 3 additional risk classification models.
PRISM-pSOFA-d2 combination summed up the scores from PRISM and p-SOFA-d2 and was continuous in nature and ranged in value from 5 to 65; where binary (Bin-PRISM-pSOFAd2) classifications where low vs high and ternary (Tri-PRISM-pSOFAd2) classifications were low vs moderate vs high.
The 3 additional risk classification models included:
· ternary model for PRISM scores (low risk: score ≤14; moderate risk: score 15-24; high risk: score ≥ 25) named tri-PRISM,
· ternary model for pSOFA-d2 scores (low risk: score ≤4; moderate risk: score 5-9; high risk: score ≥ 10), named tri-pSOFAd2
· A continuous risk stratification model that added the scores from tri-PRISM and tri-pSOFAd2 to a new ternary score classifying the administration of pressors and/or blood products (0 if neither, 1 if only one of them, and 2 if both). This combination score is called the “med-score”.
Figure 1: Receiver Operator Characteristic (ROC) curves for various prognostic scoring tools