Quality Improvement/Patient Safety 3
Session: Quality Improvement/Patient Safety 3
039 - Understanding Disparities in Post-Operative Respiratory Failure for Hospitalized Children: A Multi-site, Qualitative Study
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 39.6610
Latasha N. Easter, Children's National Health System, Upper Marlboro, MD, United States; Amina Touma, Children's National Health System, Washington, DC, United States; Pamela S.. Hinds, Children's National Health System, Silver Spring, MD, United States; Gabrina Dixon, Children's National Health System, Washington, DC, United States; Maranda C. Ward, The George Washington University School of Medicine and Health Sciences, Washington, DC, United States; Sunitha V. Kaiser, University of California, San Francisco, School of Medicine, San Francisco, CA, United States; Kavita Parikh, Children's National Health System, Washington DC, DC, United States

Latasha N. Easter, MD (she/her/hers)
Hospital Medicine Fellow
Children's National Health System
Upper Marlboro, Maryland, United States
Presenting Author(s)
Background: Disparities in preventable safety events have been identified for Black and Hispanic children, indicating a need for targeted interventions. Post-operative respiratory failure has reported disparities and complex drivers.
Objective: For post-operative respiratory failure events to: (1) identify and compare clinical processes and equity efforts between hospitals with lower and higher disparities, and (2) identify drivers of disparities and potential interventions to improve them.
Design/Methods: Individual qualitative virtual interviews were conducted via videoconference across 4 different children’s hospitals. We included quality and safety leaders, and front-line surgeons, intensivists, nurses, and respiratory therapists involved in peri-operative care (pre-operative, operative, and post-operative). Hospital-level disparities were identified using the Inpatient Essentials database (2021-23), restricting to hospitals that had > 25 total safety events and >12 patients in all racial and ethnic subgroups. Our interview guide was developed using the Systems Engineering Initiative for Patient Safety (SEIPS) model and a disparity framework by Flores et. al. A qualitative expert conducted and transcribed the interviews, and descriptive sematic content analysis consensus coding was done to identify themes.
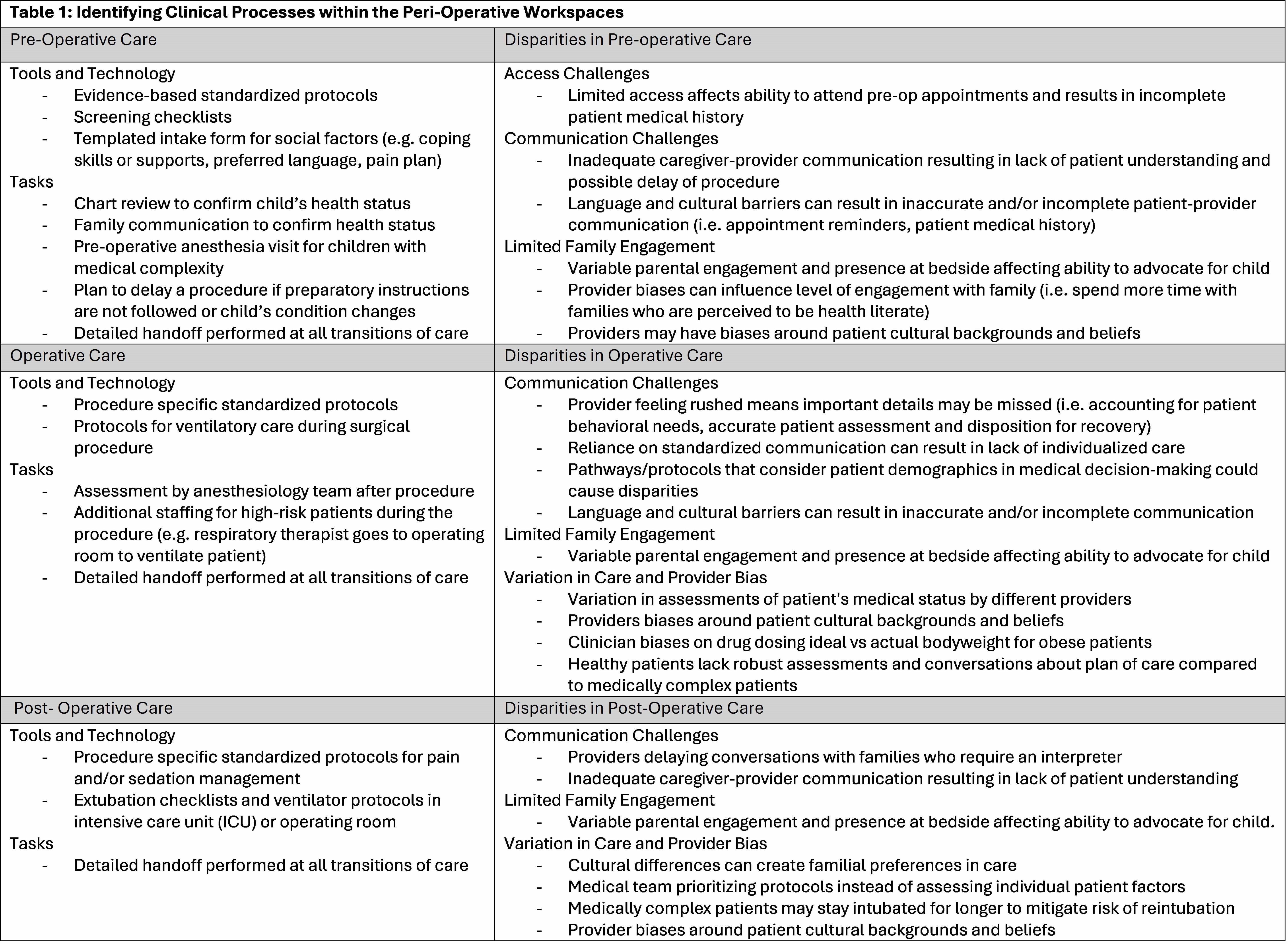
Results: Sixteen interviews were conducted with participants from 4 hospitals (3-5 interviews/hospital), including 8 physicians, 4 nurses, 3 respiratory therapists, and 1 statistician (from quality and safety team). In each peri-operative period (Table 1), clinical processes specifically tasks, tools, and technologies involved in clinical workflows were identified. Organizational equity efforts included identified leadership and team focusing on disparities with institutional knowledge of this team, hospital resources to address disparities, and training to increase awareness of personal biases. Potential drivers of disparities were identified, including challenges in care access, communication, family engagement, variation of care, and provider bias. Conversely, some leaders did not see how disparities could arise within the peri-operative space.
Conclusion(s): We identified several potential drivers and interventions to improve disparities in post-operative respiratory failure, a preventable, patient-centered safety event with high morbidity. We also illustrate a rigorous process for pairing quality/safety and equity efforts in other areas of focus.
Table 1
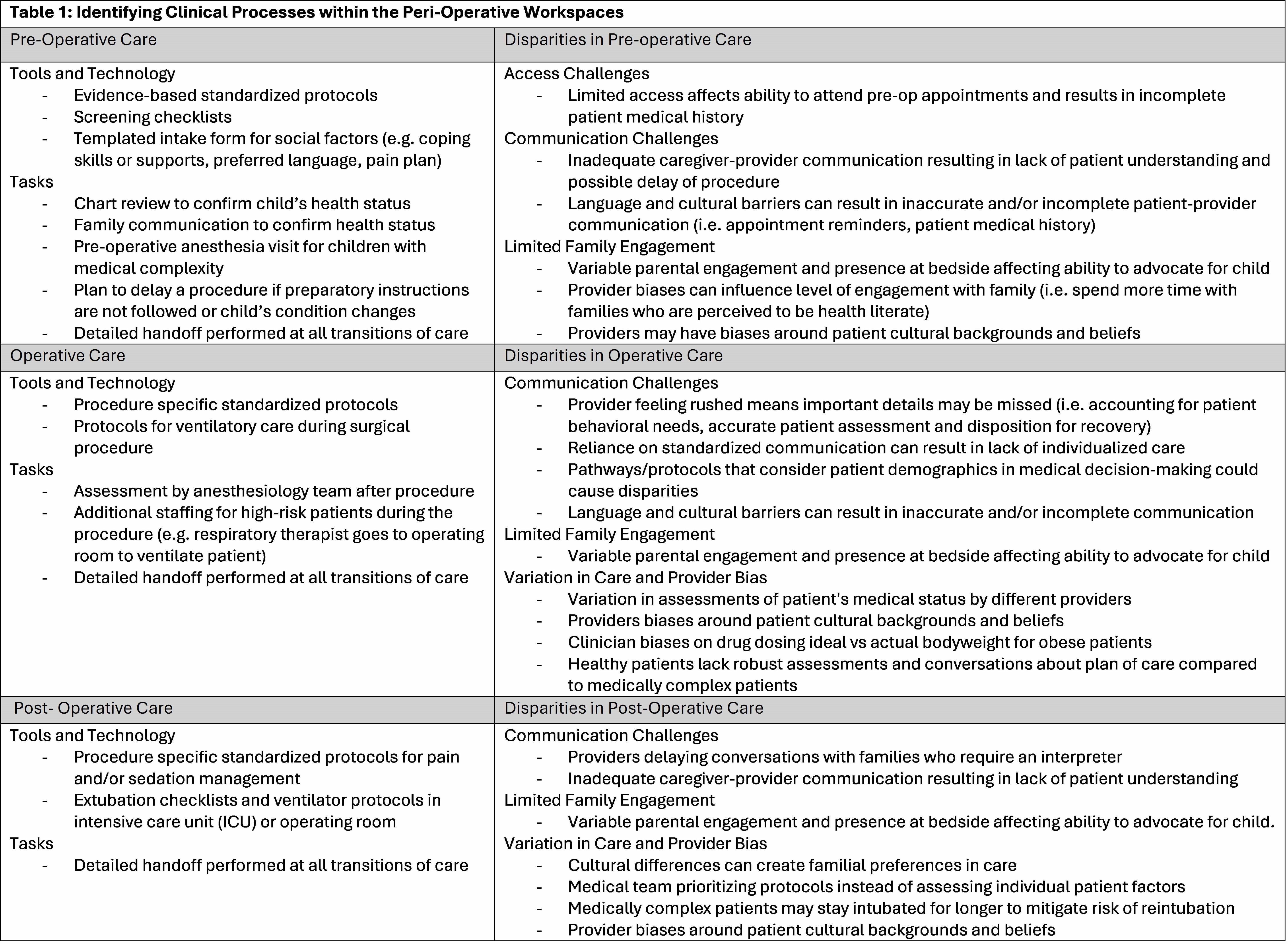
Table 1