Allergy, Immunology, and Rheumatology 2
Session: Allergy, Immunology, and Rheumatology 2
658 - Trends and Contemporary Epidemiology of Mortality Related to Primary Immunodeficiency Diseases in Children and Adults the United States, 2015-2022
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 658.6558
Ernestina Hansen-Sackey, Valley Children's Healthcare, Madera, CA, United States; Fredrick Dapaah-Siakwan, Valley Children's Healthcare, Fresno, CA, United States

Ernestina Hansen-Sackey, MD MSC (she/her/hers)
Pediatric Resident Physician
Valley Children's Healthcare
Madera, Texas, United States
Presenting Author(s)
Background: Primary Immunodeficiency Diseases (PIDD) constitute a large burden of morbidity in affected patients. There is lack of data on recent trends of population-level PIDD-related mortality.
Objective: We described the population-based temporal trends, recent epidemiology, and racial/ethnic differences in mortality related to PIDD in the United States from 2015 to 2022.
Design/Methods: We performed a retrospective, serial cross-sectional analysis of national death certificate data from the CDC WONDER website from 2015-2022. We included all deaths with PIDD (ICD-10 codes D71, D80 - D84) listed as a contributing cause of death regardless of the underlying cause of death. The exposure was the year of death. Outcomes were changes in the PIDD-related age-adjusted mortality rate (AAMR), overall, and stratified by age, gender, race/ethnicity, and census region. The AAMR was expressed as per 1,000,000 population. Differences between subgroups were evaluated with Mann-Whitney U or ANOVA as appropriate. Linear regression and correlation coefficient (R) were used to evaluate temporal trends and P< 0.05 defined statistical significance.
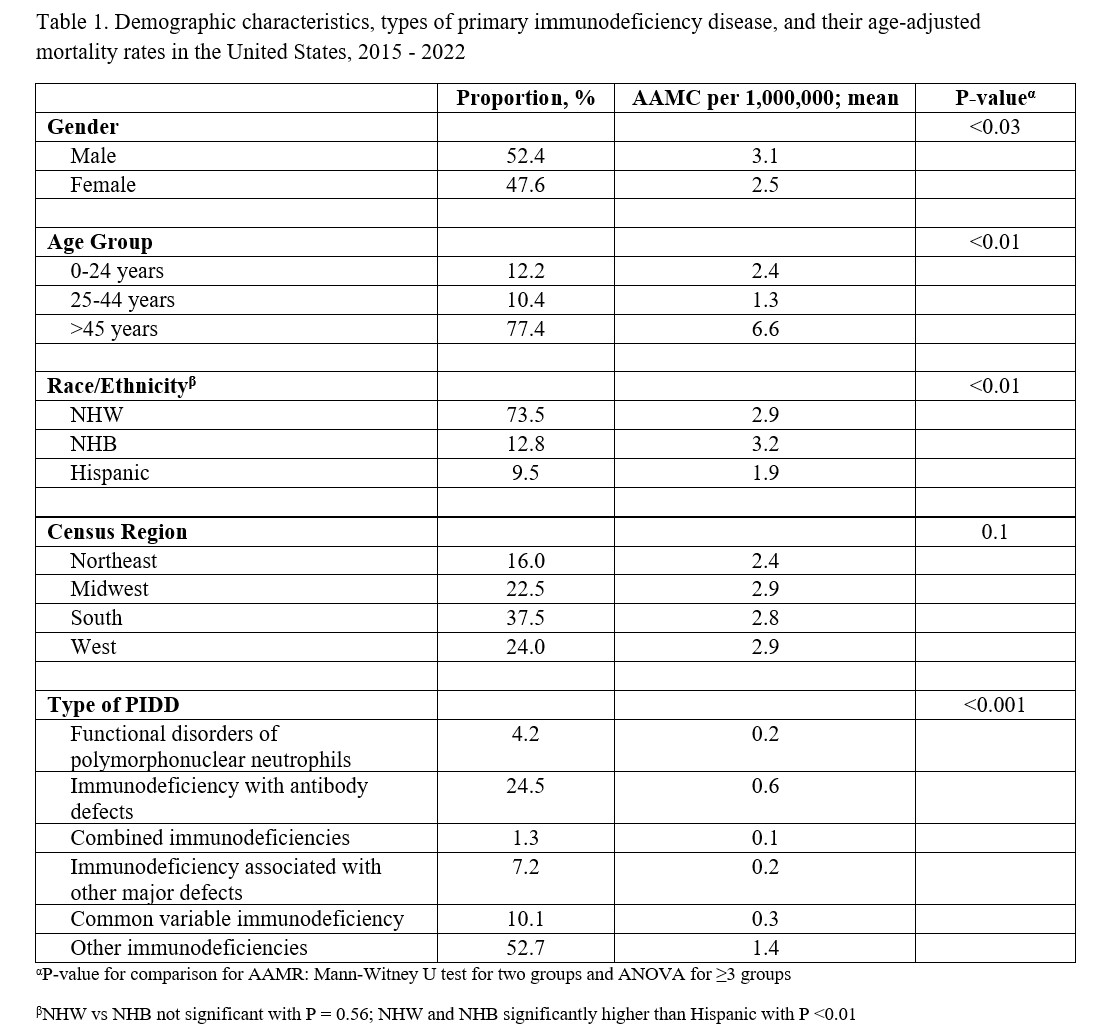
Results: Out of 2.6 billion people, there were 8,208 PIDD-related deaths (AAMR 2.8 per 1,000,000). Of the PIDD-related deaths, the majority were male, aged ≥45 years, of Non-Hispanic White (NHW) race, and more likely to have unspecified other immunodeficiencies and immunodeficiency with antibody defect [Table 1]. As shown in Table 1, the AAMR was higher in males (3.1 vs 2.5 in females, P< 0.03), and those aged ≥45 years (6.6 vs 1.3 in ages 25-44 and 2.4 in ages 0-24 years, P< 0.01) and those with other unspecified immunodeficiencies (1.4 vs 0.1 – 0.6 in the other PIDD, P< 0.001). The PIDD-related AAMR increased significantly from 2.5 to 3.5, P< 0.01, R= 0.83) [Figure 1]. Similarly, there was a statistically significant increase in the AAMR in males (3 to 3.9, P=0.02, R = 0.78), females (2.1 to 3.2, P < 0.02, R = 0.84), NHW (2.5 to 3.8, P< 0.01, R = 0.86), and Hispanics (1.7 to 2.8; R = 0.84; P< 0.01). However, there was no significant change in NHB (3.5 to 3.6, P = 0.98; R = 0) and all age groups except in those aged ≥65 years which showed a significant increase from 8.2 to 13.9 (P < 0.001; R = 0.94).
Conclusion(s): The overall PIDD-related AAMR increased during the study period and in several demographic subgroups especially those aged < 65 years. Unspecified immunodeficiencies and immunodeficiency with antibody defects contributed mostly to PIDD deaths. This data can enhance awareness and guide healthcare resource allocation towards early recognition and mitigating PIDD-related mortality.
Table 1.
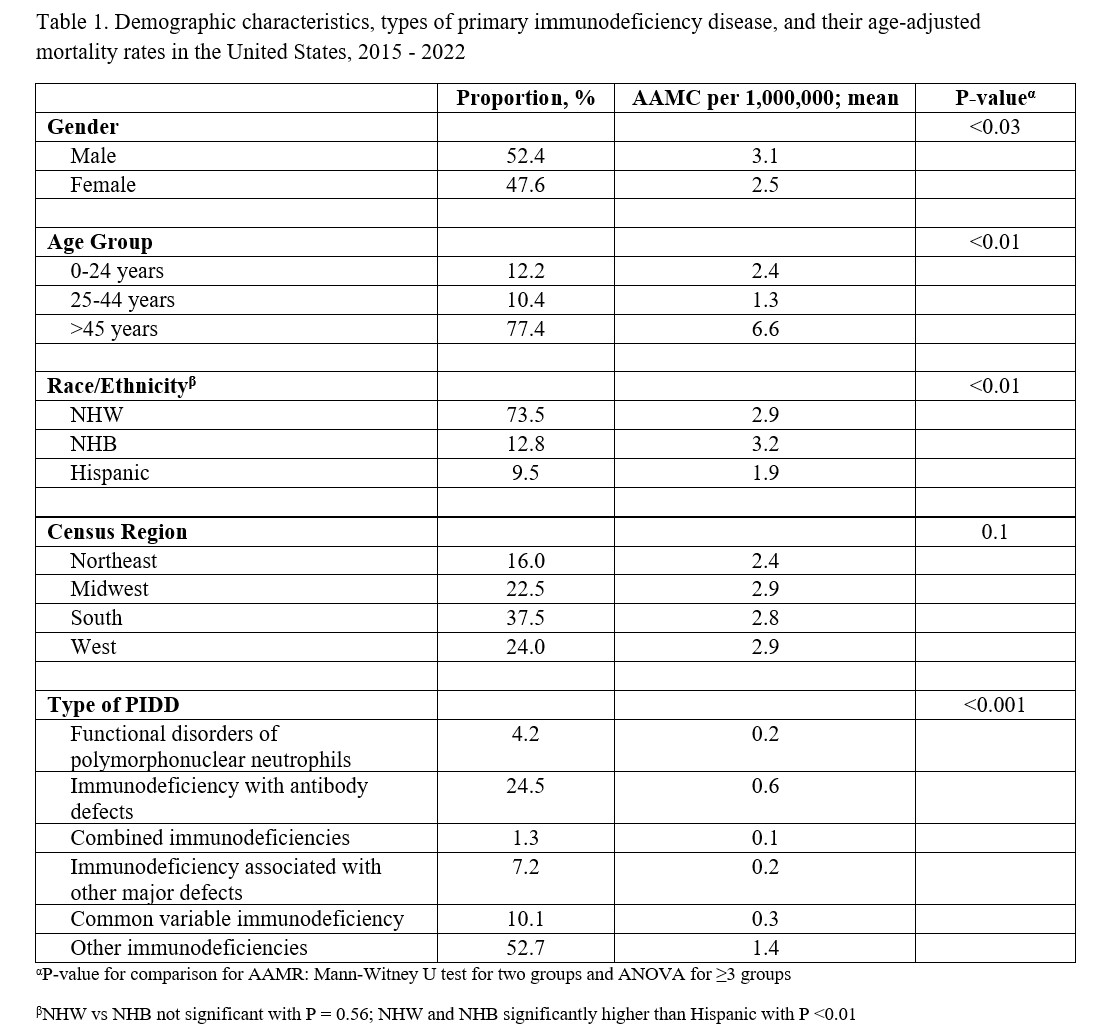 Demographic characteristics, types of primary immunodeficiency disease, and their age-adjusted mortality rates in the United States, 2015 - 2022
Demographic characteristics, types of primary immunodeficiency disease, and their age-adjusted mortality rates in the United States, 2015 - 2022Figure 1
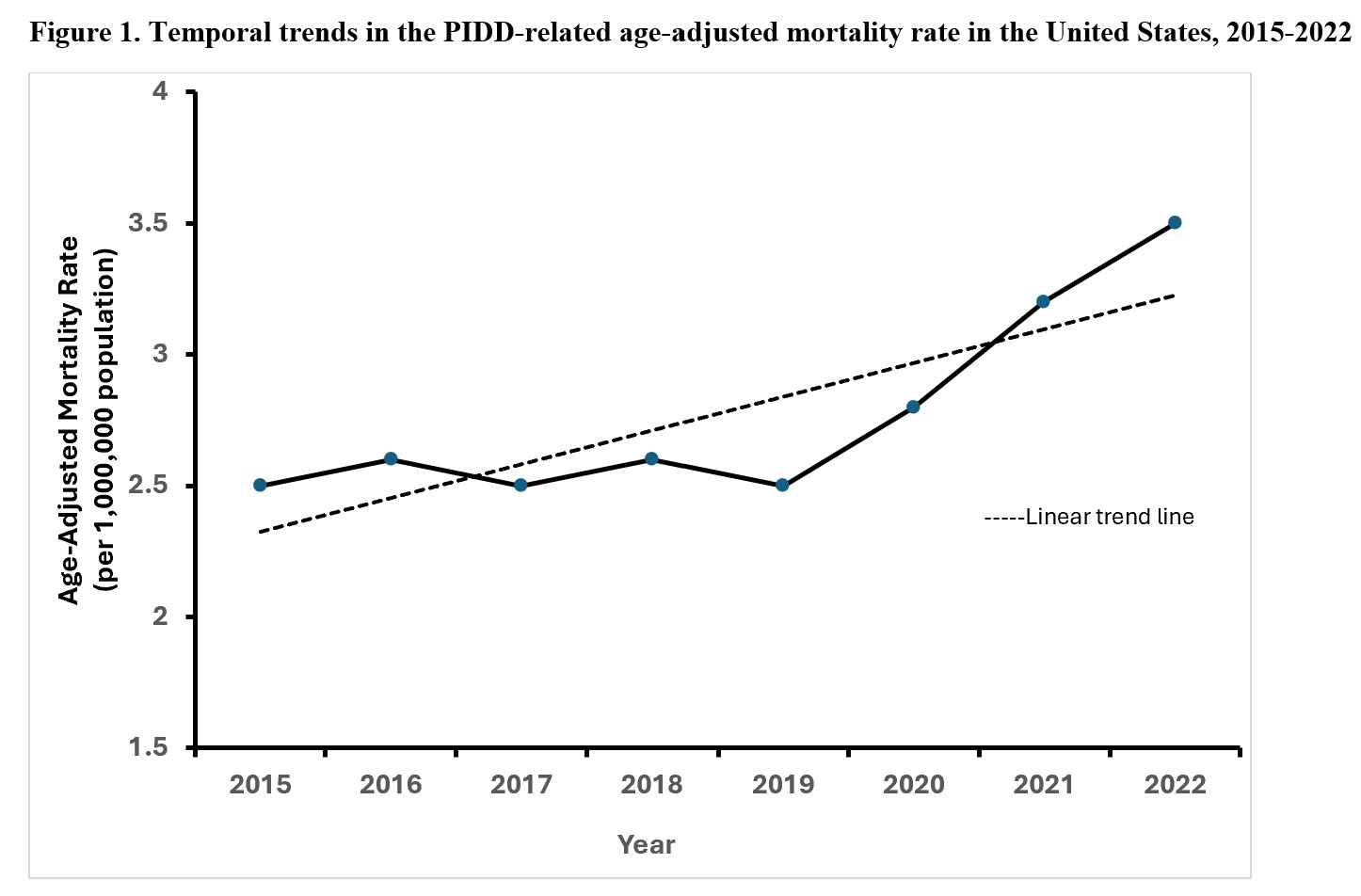 Temporal trends in the PIDD-related age-adjusted mortality rate in the United States, 2015-2022
Temporal trends in the PIDD-related age-adjusted mortality rate in the United States, 2015-2022Table 1.
 Demographic characteristics, types of primary immunodeficiency disease, and their age-adjusted mortality rates in the United States, 2015 - 2022
Demographic characteristics, types of primary immunodeficiency disease, and their age-adjusted mortality rates in the United States, 2015 - 2022Figure 1
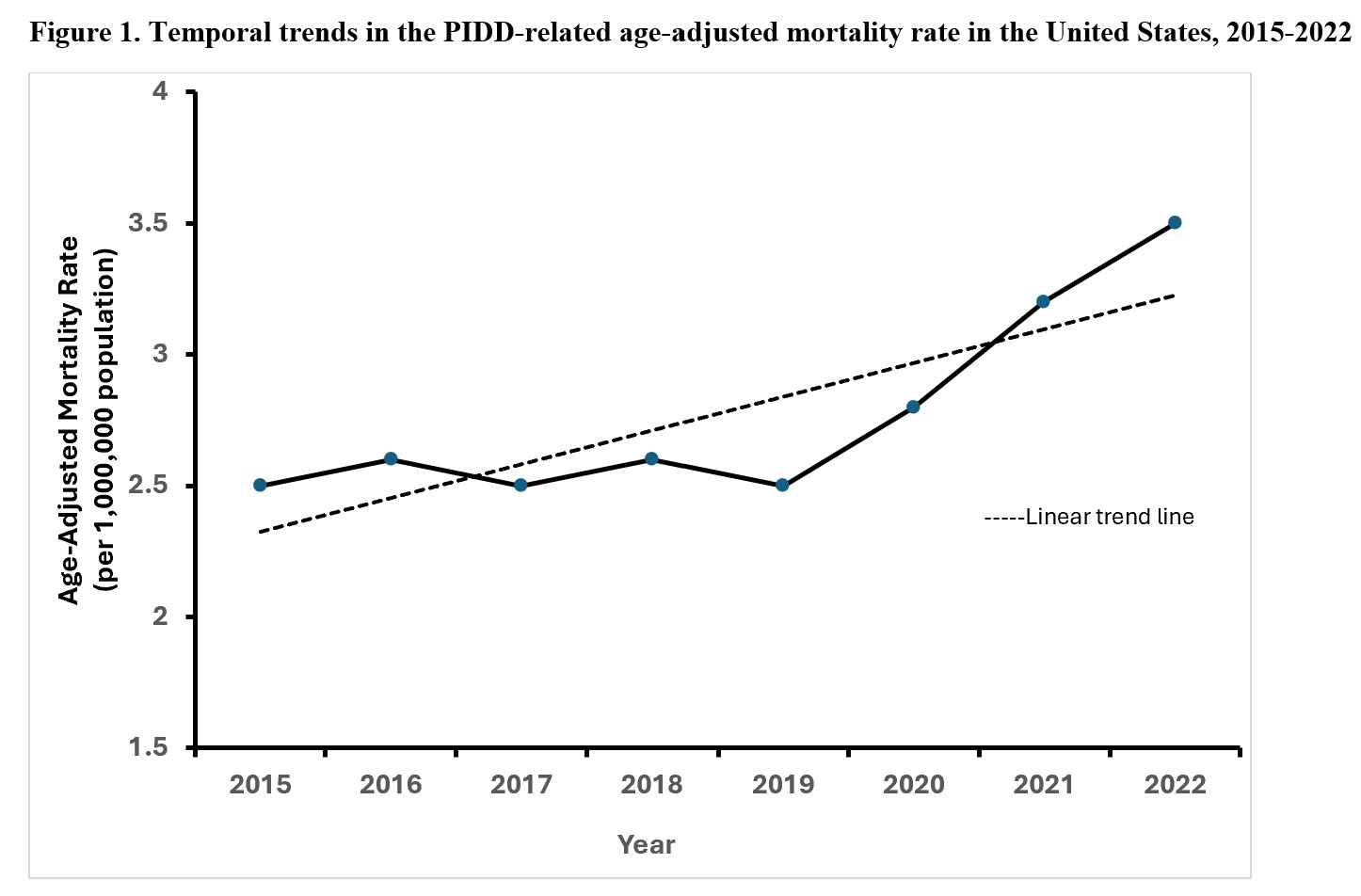 Temporal trends in the PIDD-related age-adjusted mortality rate in the United States, 2015-2022
Temporal trends in the PIDD-related age-adjusted mortality rate in the United States, 2015-2022
