Neonatal Quality Improvement 1
Session: Neonatal Quality Improvement 1
051 - A Quality Improvement Study to Reduce Central Line-Associated Bloodstream Infections (CLABSI) in A Neonatal Intensive Care Unit (NICU) in A Tertiary Care Hospital in Karamsad, Gujarat.
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 51.4001
Bhushan Bhaskarrao. Korde, Pramukhswami Medical College Karamsad Anand Gujarat 388325, Anand, Gujarat, India; Dipen V. Patel, Shree Krishna Hospital, Pramukhswami Medical College, Bhaikaka University, Gujarat, India, Anand, Gujarat, India; Reshma Pujara, Shree Krishna Hospital, Bhaikaka University, Anand, Gujarat, India; Somashekhar M.. Nimbalkar, Bhaikaka University, Karamsad, Gujarat, India

Somashekhar M. Nimbalkar, n/a
Professor
Bhaikaka University
Karamsad, Gujarat, India
Presenting Author(s)
Background: Sick neonates in the NICU frequently need insertion of central lines, placing them at high risk of contracting a CLABSI. Infections increase the risk of morbidity, mortality, medical costs, and hospital length of stay in the NICU.
Objective: Improve adherence to the CLABSI maintenance Care bundle checklist from 70 % to 100% and reduce CLABSI rate from ~ 10 per 1000 central line days to < 5 per 1000 central line days in the NICU.
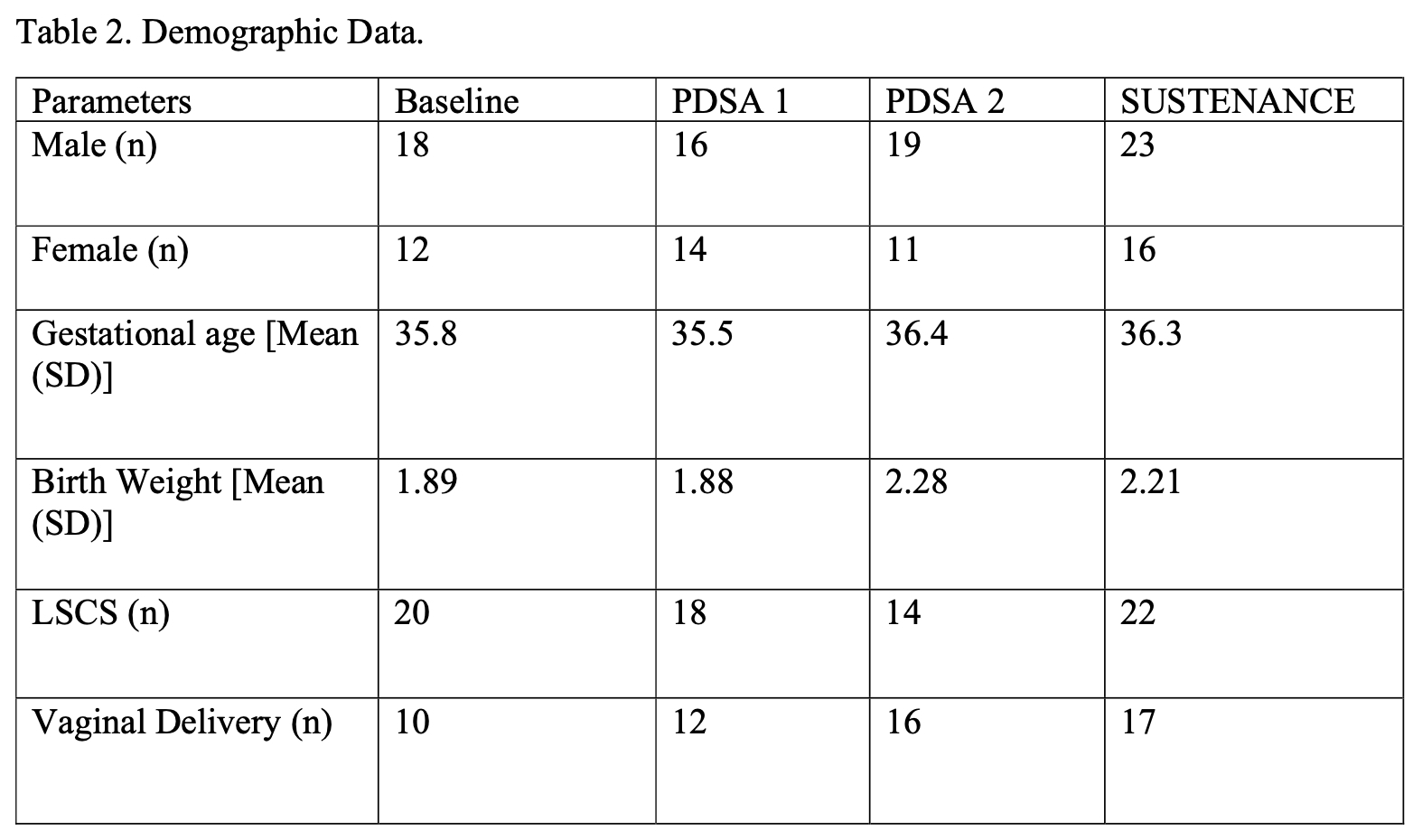
Design/Methods: This quality improvement study was conducted at the NICU of a tertiary care teaching institute over 13 months using the Plan-Do-Study-Act (PDSA) principle. All the newborns requiring central line placement were included. CLABSI maintenance care bundle checklist was utilized, and baseline data was collected between Jun & Oct 2023. Potential barriers to adherence to the central line-associated bloodstream infections maintenance care bundle checklist were identified using fishbone analysis (Figure 1). Possible interventions were identified, introduced & then evaluated by multiple PDSA cycles (Table 1) The first intervention was documentation & real-time monitoring of adherence to CLABSI maintenance care bundles by staff nurses on duty. The second intervention was during each duty shift infection control champion educated & empowered staff nurses and resident doctors. Data was again collected to check sustenance.
During all the phases, data was transcribed to an Excel file daily. Weekly assessment of this data was presented in the joint regular meetings. These meetings were convened by two consultant neonatologists involving all the stakeholders [senior residents (i.e., recently passed MD exam), staff nurses, and resident doctors] every week during the implementation phase to appraise everyone about the current situation and to discuss change ideas to be implemented in the next PDSA cycle. No new interventions were done in the sustenance phase. The analysis was performed using STATA (14.2).
Results: Adherence to the CLABSI maintenance care bundles checklist improved significantly from 65 % to 100% in PDSA cycle 2 which stabilized to 99% in the sustenance phase. The Mean (SD) CLABSI maintenance care bundles checklist improved significantly in all PDSA cycles and remained stable during sustenance (P < 0.001). CLABSI rate of 13.24 per 1000 central line days at the Baseline improved to 0 in PDSA cycle 2 and remained under control (4.85) in the sustenance phase.
Conclusion(s): The current study resulted in increased CLABSI care bundle adherence and a reduction in CLABSI rate per 1000 central line days.
Figure 1: Fishbone Analysis
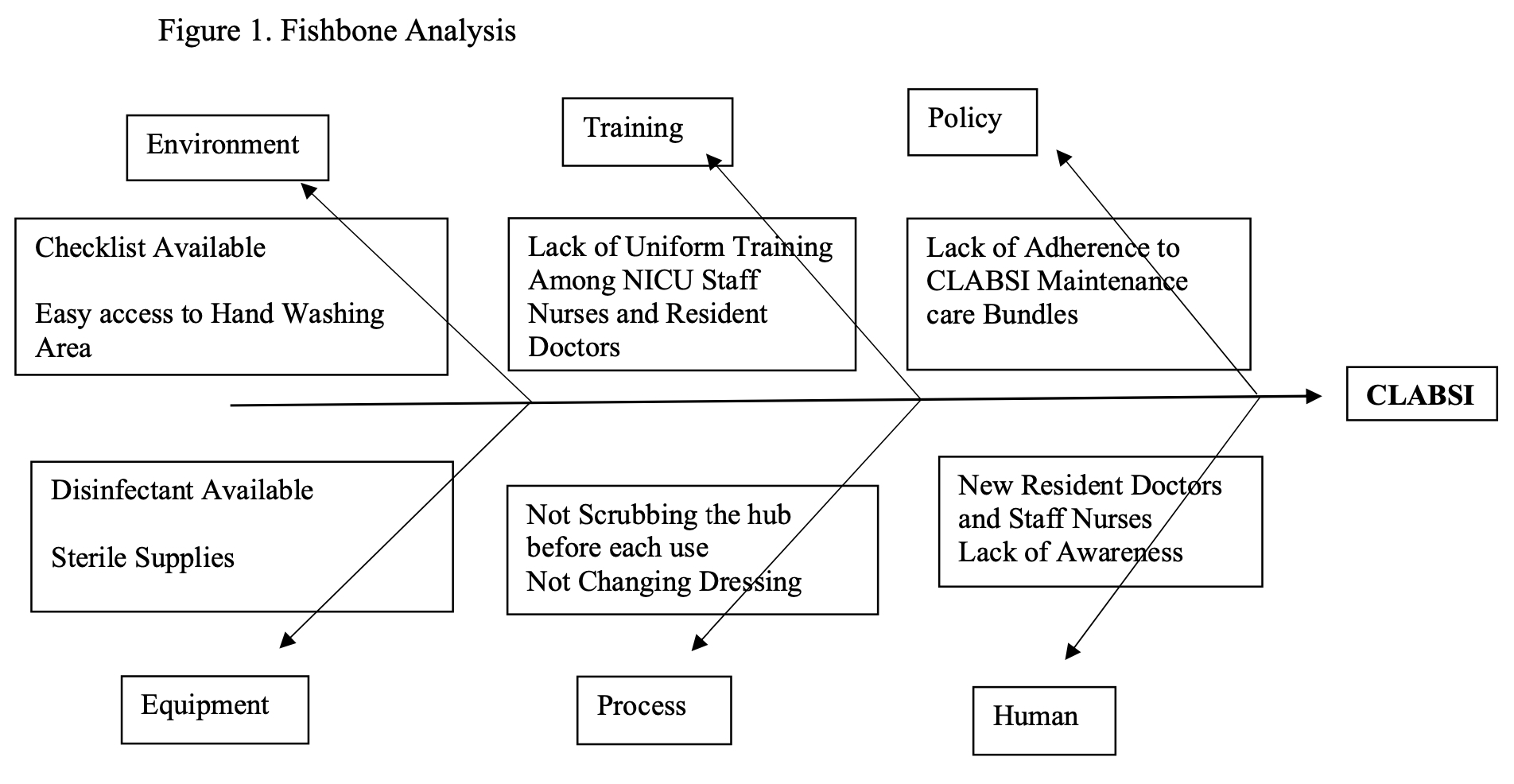
Table 1: PDSA cycles
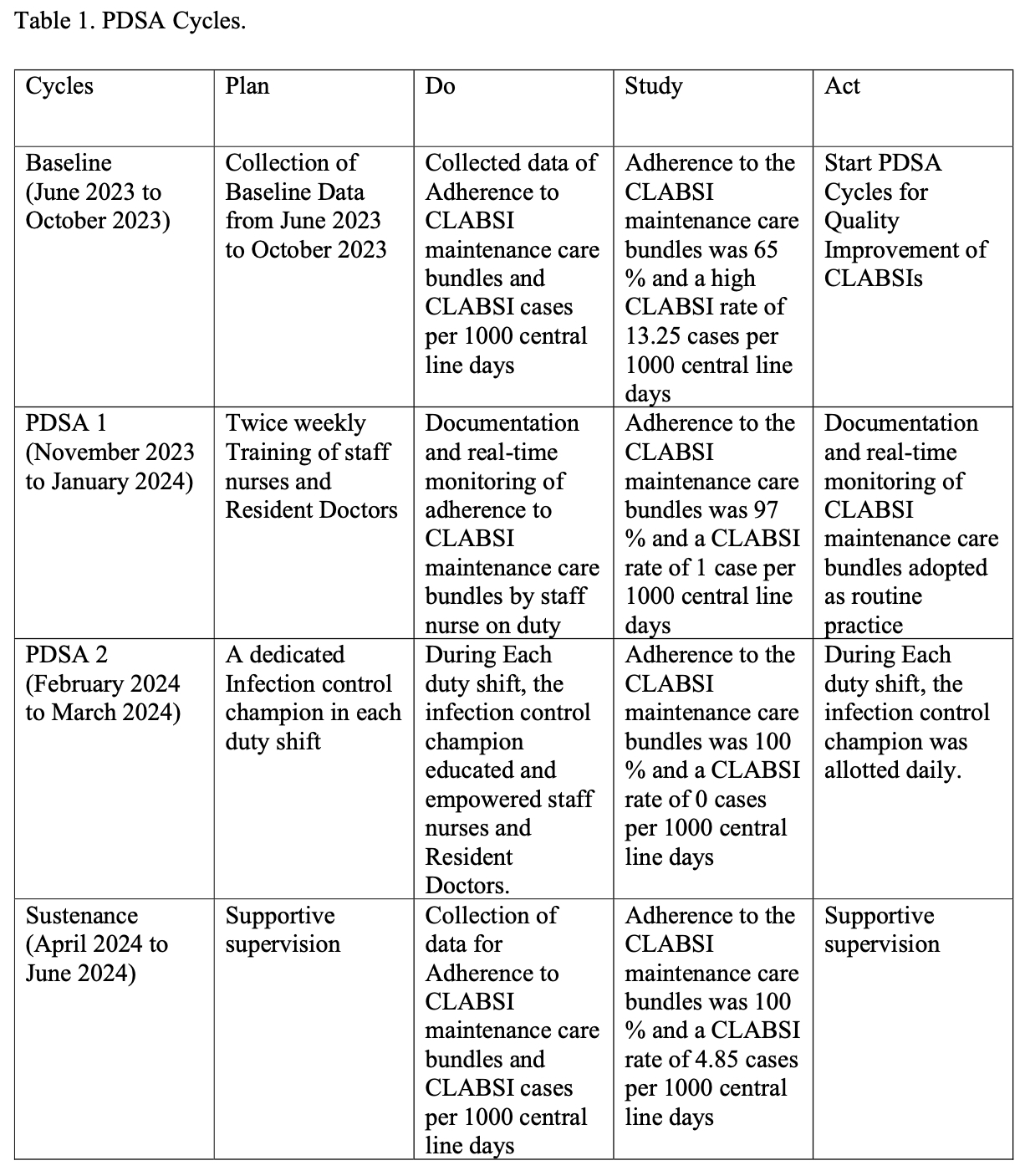
Table 2: Demographic Data