Neonatal General 2: Neurology
Session: Neonatal General 2: Neurology
318 - Enteral Nutrition in Neonates with Hypoxic Ischemic Encephalopathy: Correlation with Short Term Outcomes
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 318.5002
Ahreen Allana, University of Texas Southwestern Medical School, Dallas, TX, United States; Rachel Clark, University of Texas Southwestern Medical School, Dallas, TX, United States; Emily Bordier, University of Texas Southwestern Medical School, Dallas, TX, United States; Lina Chalak, UTSW, Dallas, TX, United States; Rachel L.. Leon, University of Texas Southwestern Medical School, Dallas, TX, United States
- AA
Ahreen Allana, MD (she/her/hers)
Fellow
University of Texas Southwestern Medical School
Dallas, Texas, United States
Presenting Author(s)
Background: Neonates with hypoxic ischemic encephalopathy (HIE) are at theoretical risk of feeding intolerance in the first days of life. For those receiving therapeutic hypothermia (TH), enteral nutrition is typically withheld due to this concern. However, recent evidence suggests that infants who receive enteral feeds during TH tolerate them well and achieve full enteral nutrition sooner, leading to a shorter hospital length of stay (LOS) compared to infants who are not fed during TH. Algorithms to guide feeding initiation in neonates with HIE receiving TH may improve safety and medical team comfort with feeding during TH, and ultimately improve short term outcomes.
Objective: To determine the correlation between current enteral feeding practices and short term outcomes in infants with moderate or severe HIE.
Design/Methods: This was a retrospective cohort study of infants born at >35 weeks gestation with moderate or severe HIE who underwent TH between 2009-2023. Uniformly, enteral feeds were introduced after completion of TH and rewarming. We evaluated the correlation between short term outcomes and enteral feeding practices, including day of life (DOL) of enteral nutrition initiation, attainment of full enteral feeds, and initiation of oral feeds. We also compared differences in feeding and feeding-related outcomes between infants with moderate versus severe HIE.
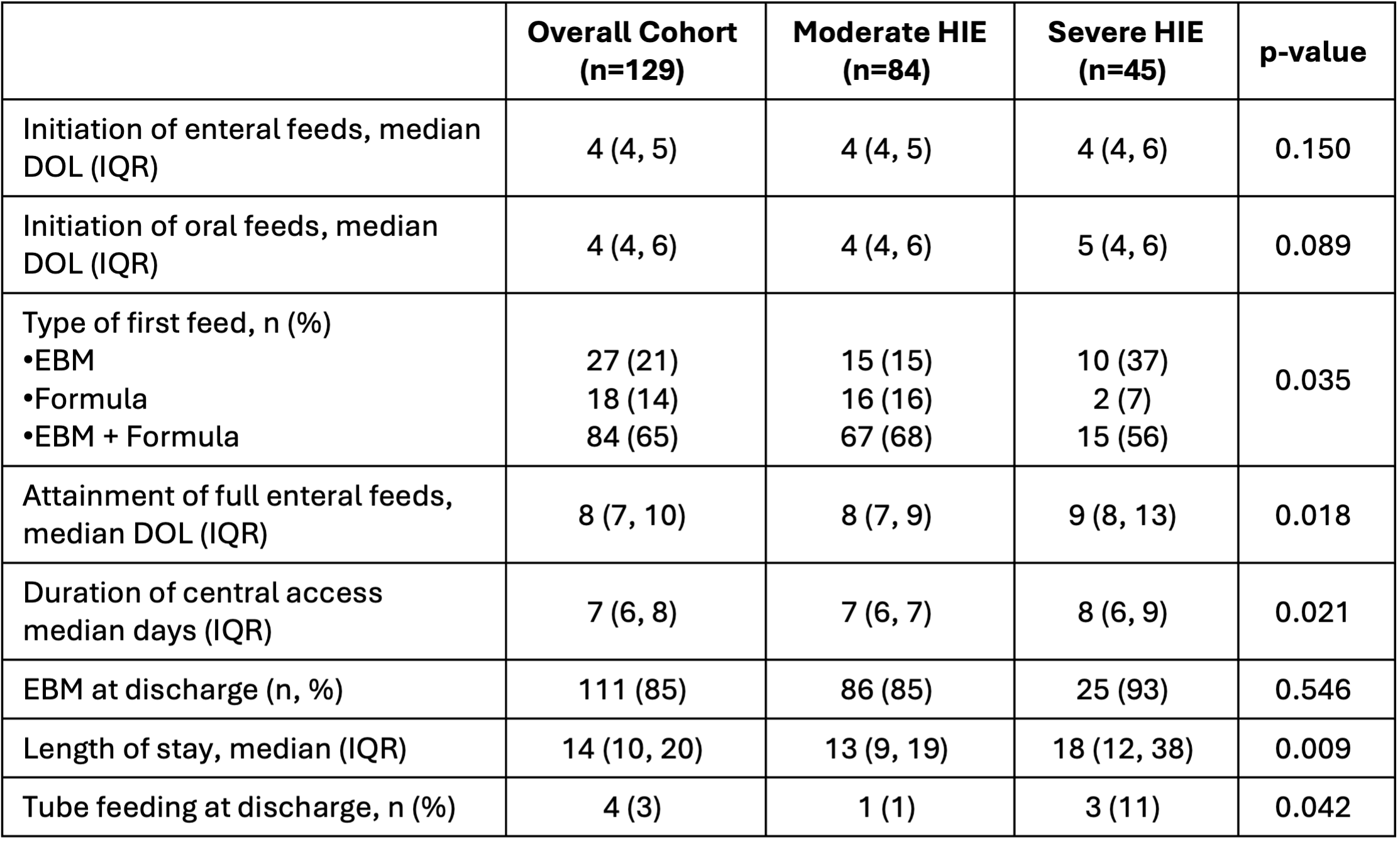
Results: The cohort of 129 infants included 84 with moderate HIE and 45 with severe HIE. Enteral nutrition was initiated at a median DOL 4 (IQR 4, 5) and was not significantly different between infants with moderate versus severe HIE. Full enteral feeds were reached at a median DOL 8 (IQR 7, 10). Those with moderate HIE achieved full feeds sooner than those with severe HIE (Table 1). The DOL of enteral nutrition initiation was moderately correlated with both duration of central venous access as well as LOS (p < 0.0001 and p < 0.0001, respectively; Figure 1A, B). DOL to attain full enteral nutrition was strongly correlated with both central access duration and LOS (p < 0.0001 and p < 0.0001, respectively; Figure 1C, D).
Conclusion(s): In neonates with HIE, time to initiate enteral nutrition and time to attain full enteral feeds correlates with duration of central access and hospital LOS. Earlier initiation of enteral feeding may improve short term outcomes for neonates with HIE.
Comparison of outcomes associated with enteral nutrition in infants with moderate vs. severe HIE
Correlation Between Enteral Feeds and Short Term Outcomes
.png) In the whole cohort, the day of life when enteral feeds were initiated was moderately correlated with duration of central venous access (Panel A, Spearman 𝜌= 0.50, p <0.0001) and hospital length of stay (Panel B, Spearman 𝜌= 0.45, p <0.0001). Day of life to reach full enteral feeds was strongly correlated with duration of central venous access (Panel C, Spearman 𝜌= 0.74, p <0.0001) and hospital length of stay (Panel D, Spearman 𝜌= 0.64, p <0.0001); shaded area indicates 95% CI.
In the whole cohort, the day of life when enteral feeds were initiated was moderately correlated with duration of central venous access (Panel A, Spearman 𝜌= 0.50, p <0.0001) and hospital length of stay (Panel B, Spearman 𝜌= 0.45, p <0.0001). Day of life to reach full enteral feeds was strongly correlated with duration of central venous access (Panel C, Spearman 𝜌= 0.74, p <0.0001) and hospital length of stay (Panel D, Spearman 𝜌= 0.64, p <0.0001); shaded area indicates 95% CI.
