Neonatal/Infant Resuscitation 2
Session: Neonatal/Infant Resuscitation 2
304 - Pulmonary Blood Flow Changes at Birth in Spontaneously Breathing Versus Mechanically Ventilated Lambs
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 304.6294
Indya M. Davies, Hudson Institute of Medical Research, Clayton, Victoria, Australia; Valerie Zahra, Hudson Institute of Medical Research, Clayton, Victoria, Australia; Alison Thiel, Hudson Institute of Medical Research, clayton, Victoria, Australia; Douglas Blank, Dept of Paediatrics, Monash University and Monash Newborn, Port Melbourne, Victoria, Australia; Graeme Polglase, Monash University, Melbourne, Victoria, Australia; Stuart B. Hooper, Monash University, Black Rock, Victoria, Australia; Kelly J. Crossley, The Ritchie Centre, Clayton, Victoria, Australia

Indya M. Davies, BSc(Hons), PhD (she/her/hers)
PhD Student
Hudson Institute of Medical Research
Clayton, Victoria, Australia
Presenting Author(s)
Background: Lung aeration at birth triggers the increase in pulmonary blood flow (PBF) and cardiovascular changes essential for postnatal survival. These haemodynamic changes have largely been described in intubated, anaesthetised and mechanically ventilated (MV) lambs, however it is unknown whether these changes are similar in unanaesthetised, spontaneously breathing (SB) newborn lambs. We hypothesised that the increase in PBF at birth would be similar in MV and SB lambs, but that SB lambs would take longer to achieve this increase after birth.
Objective: To compare the haemodynamic transition at birth in MV versus SB near-term newborn lambs.
Design/Methods: We retrospectively analysed data from instrumented near term lambs delivered by caesarean section (CS) at 139/147 days gestation that were either MV or SB from birth. MV lambs (n=8) underwent instrumentation surgery to implant blood flow probes and catheters immediately prior to CS delivery under maternal general anaesthesia. SB lambs (n=9) were instrumented at 137 days before they were delivered at 139 days by CS under maternal spinal anaesthesia. MV lambs were ventilated to a tidal volume of 7 mL/kg. SB lambs were provided with oxygen via nasal cannula (if required) to stimulate spontaneous breathing after delivery. PBF, cerebral blood flow (CBF), arterial blood pressure, heart rate and respiratory rate were measured continuously during the first hour after birth. Data (mean±SD) were tested for normality and compared using mixed-model analysis (GraphPad Prism).
Results: Both groups had similar PBF (per kg body weight) at the onset of ventilation or spontaneous breathing (19.2±12.4 vs. 22.2±14.1 mL/min/kg, p=0.64) and spent a similar time being ventilated or breathing prior to umbilical cord clamping (4.0±0.8 vs. 7.5±5.4 mins, MV vs. SB, p = 0.17). At cord clamping, PBF was not different between groups (70.6±27.4 vs. 55.7±23.2 mL/min/kg, MV vs. SB, p=0.24; Fig 1A). Following cord clamping, the increase in PBF over time was similar in both groups (p=0.17; Fig 1A) and reached a similar peak (120.0±13.6 vs. 110.0±6.5 mL/min/kg, p=0.50; Fig 1B). However, MV lambs required significantly fewer inflations than breaths (684±314 vs. 1390±655, p=0.01; Fig 1C) and took less time (13.8±2.3 vs. 26.2±3.0 mins, p=0.006; Fig 1D) to achieve peak PBF compared to SB lambs. SB lambs had higher CBF (p=0.004), heart rate (p=0.04) and arterial blood pressure (p=0.03) after umbilical cord clamping compared to MV lambs.
Conclusion(s): MV and SB lambs experience the same increase in PBF at the time of birth, however MV lambs achieved this increase more efficiently that SB lambs.
Fig 1. Increases in pulmonary blood flow (PBF; per kg body weight) after umbilical cord clamping (UCC) in mechanically ventilated and spontaneously breathing newborn lambs.
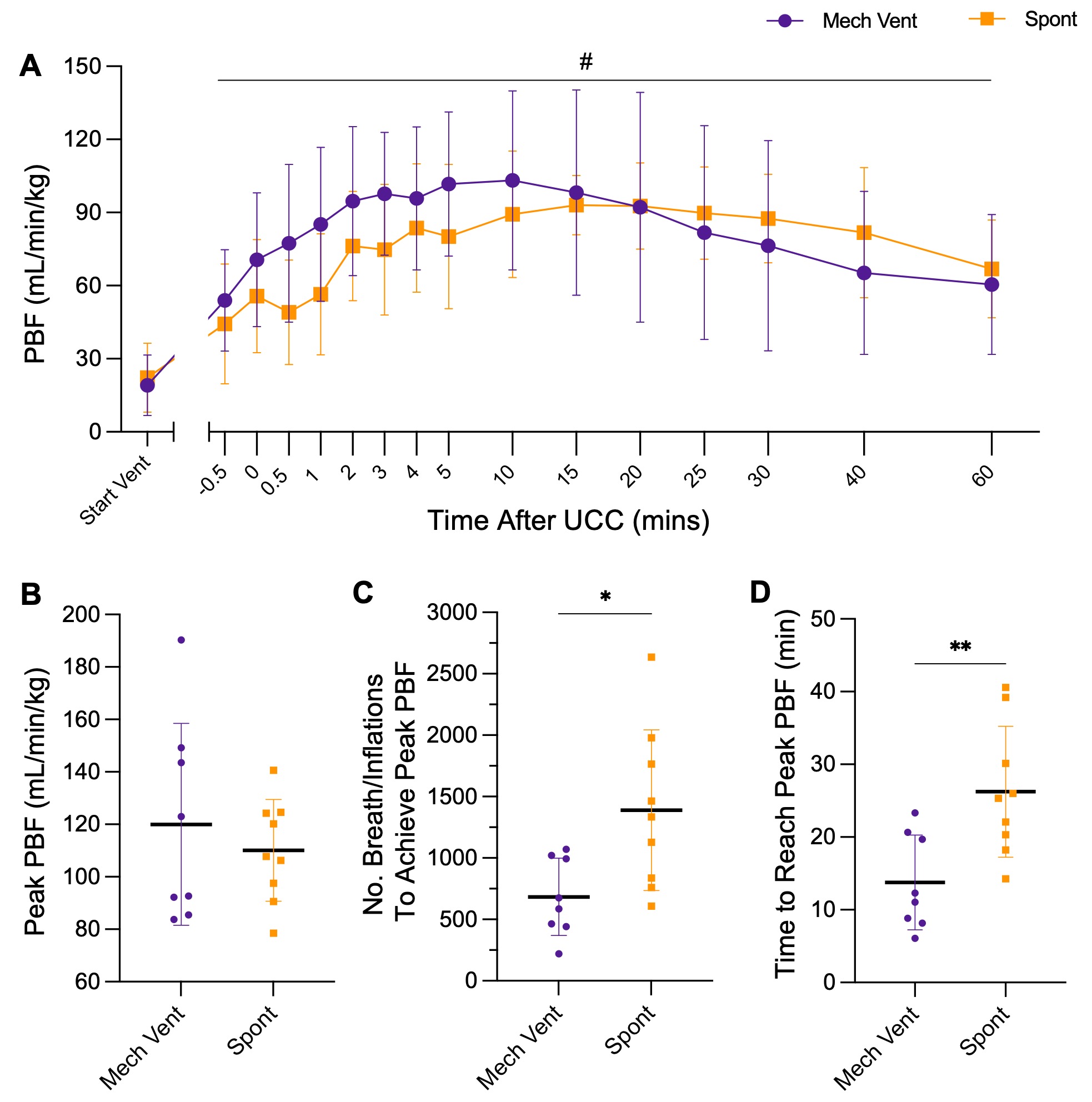 A: PBF at the onset of breathing/ventilation (Start Vent) and during the first hour after UCC. B: Peak PBF achieved after UCC. C: The number of breaths or inflations required to achieve the peak PBF after UCC. D: Time taken to achieve peak PBF after UCC. Groups were compared using mixed model analysis (A) or by unpaired t-test (B-D). Data are mean±SD. #p=0.0001, time effect. *p=0.01 and **p=0.006, Mech Vent vs. Spont.
A: PBF at the onset of breathing/ventilation (Start Vent) and during the first hour after UCC. B: Peak PBF achieved after UCC. C: The number of breaths or inflations required to achieve the peak PBF after UCC. D: Time taken to achieve peak PBF after UCC. Groups were compared using mixed model analysis (A) or by unpaired t-test (B-D). Data are mean±SD. #p=0.0001, time effect. *p=0.01 and **p=0.006, Mech Vent vs. Spont.
