Neonatal Infectious Diseases/Immunology 2: Congenital infections
Session: Neonatal Infectious Diseases/Immunology 2: Congenital infections
586 - Effect of Maternal Antibiotics Administered within Seven Days Before Delivery on Early Neonatal Mortality: A Retrospective Propensity Score-Matched Analysis
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 586.5006
Vivek Kumar, AIIMS New Delhi, New Delhi, Delhi, India; Kajal Jain, All India Institute of Medical Sciences, New Delhi, New Delhi, Delhi, India; Ramesh Agarwal, All India Institute of Medical Sciences, New Delhi, New Delhi, Delhi, India; M Jeeva Sankar, All India Institute of Medical Sciences, New Delhi, New Delhi, Delhi, India; On Behalf of Investigators of DeNIS and DH study, India, New Delhi, Delhi, India
- VK
Vivek Kumar, MD, DM (he/him/his)
Research Consultant
AIIMS New Delhi
New Delhi, Delhi, India
Presenting Author(s)
Background: There is a paucity of data regarding the role of antibiotics administered to mothers just before delivery in preventing neonatal sepsis and mortality, especially in LMICs.
Objective: To evaluate the effect of antibiotics administered to mothers within seven days before delivery on early (≤ 7 days) neonatal mortality and culture-positive sepsis.
Design/Methods: This is a retrospective propensity score (PS) matched analysis using datasets of two multicentric studies – Delhi Neonatal Infection Study (DeNIS) and District Hospital –that enrolled neonates from tertiary and secondary level hospitals, respectively, in India. Outborn neonates, multiple births, and mothers who underwent cesarean section and received antibiotics for one day were excluded. We used the 2:1 nearest neighbor PS matching using caliper width 0.1 without replacement to assess the association between the exposure and the outcome variables. The exposure was mothers receiving antibiotics within 7 days before birth or during labor (‘abx cohort’); the ‘control cohort’ did not receive antenatal or intrapartum antibiotics. The primary outcome was early neonatal mortality (within 7 days of life). Secondary outcomes were in-hospital mortality and incidence of early-onset (within 72 hours of life) culture-positive sepsis. Multivariable logistic regression was performed to examine the association between exposure and outcomes after adjusting for the confounders.
Results: Among 13204 (DeNIS: 10502, DH: 2702) neonates included for analysis, 2060 (15.6%) neonates were born to mothers who had received antenatal or intrapartum antibiotics. The propensity-matched cohort included 4474 neonates (mean gestation 35.2 weeks [SD 3.6]; 1944 [43.5%] females):1546 in the ‘abx cohort’ and 2928 in the control cohort. 158 (10.2%) in the ‘abx cohort’ died within 7 days compared to 478 (16.3%) in the other group (adjusted odds ratio [aOR] 0.66; 95% CI 0.53 to 0.82; p< 0.001). The in-hospital mortality was also lower in the ‘abx cohort’ (201 [13.4%] vs 549 [19.2%]; aOR 0.68; 95% CI 0.55 to 0.84; p< 0·001). However, the incidence of early-onset culture-positive sepsis was higher in the ‘abx cohort’ (6.0% vs 4.6%; aOR 1.4; 95% CI 1.1 to 1.9).
Conclusion(s): In this post-hoc analysis of two large Indian cohorts, neonates whose mothers had received antibiotics within 7 days before delivery had lower 7-day and in-hospital all-cause mortality despite being at higher risk of early-onset sepsis. Further research is warranted to validate and explore the implications of these findings for clinical practice.
Figure 1. Outcomes of neonates among the two groups in the whole cohort
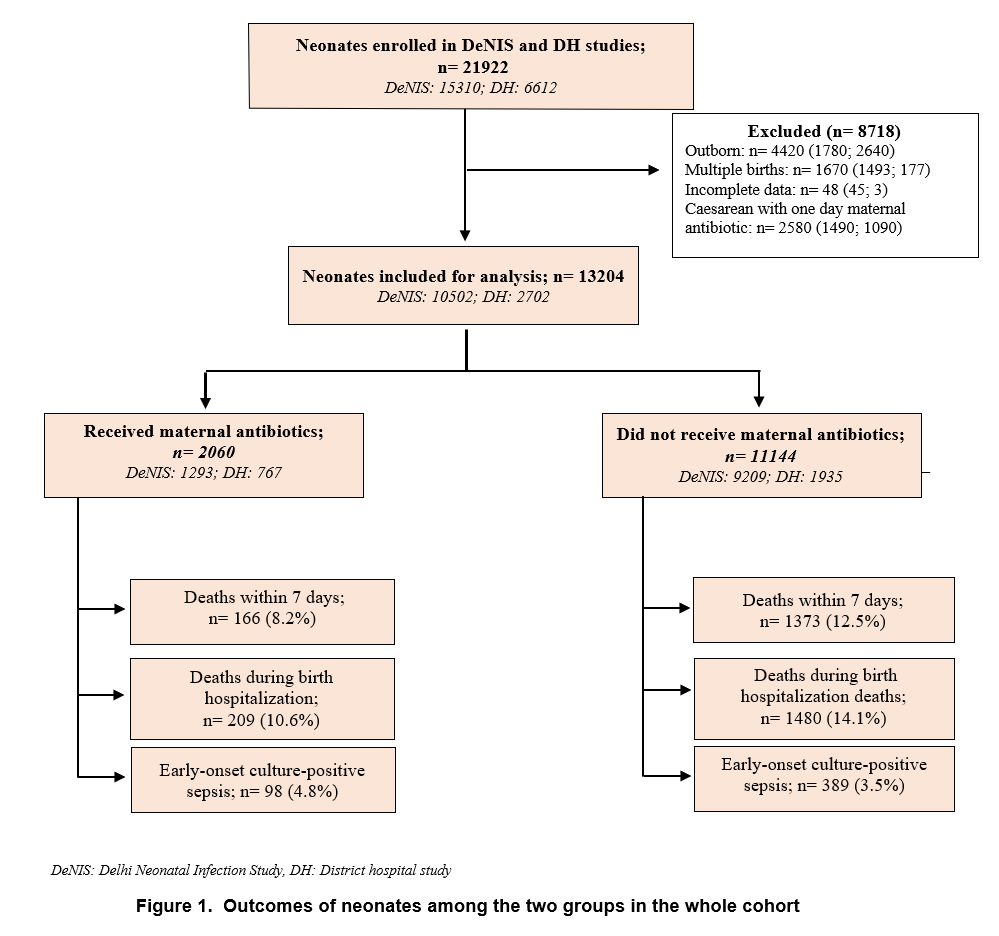 DeNIS: Delhi Neonatal Infection Study, DH: District hospital study
DeNIS: Delhi Neonatal Infection Study, DH: District hospital studyTable 1: Characteristics of mothers and neonates with and without maternal antibiotics in the two studies (DeNIS and DH)
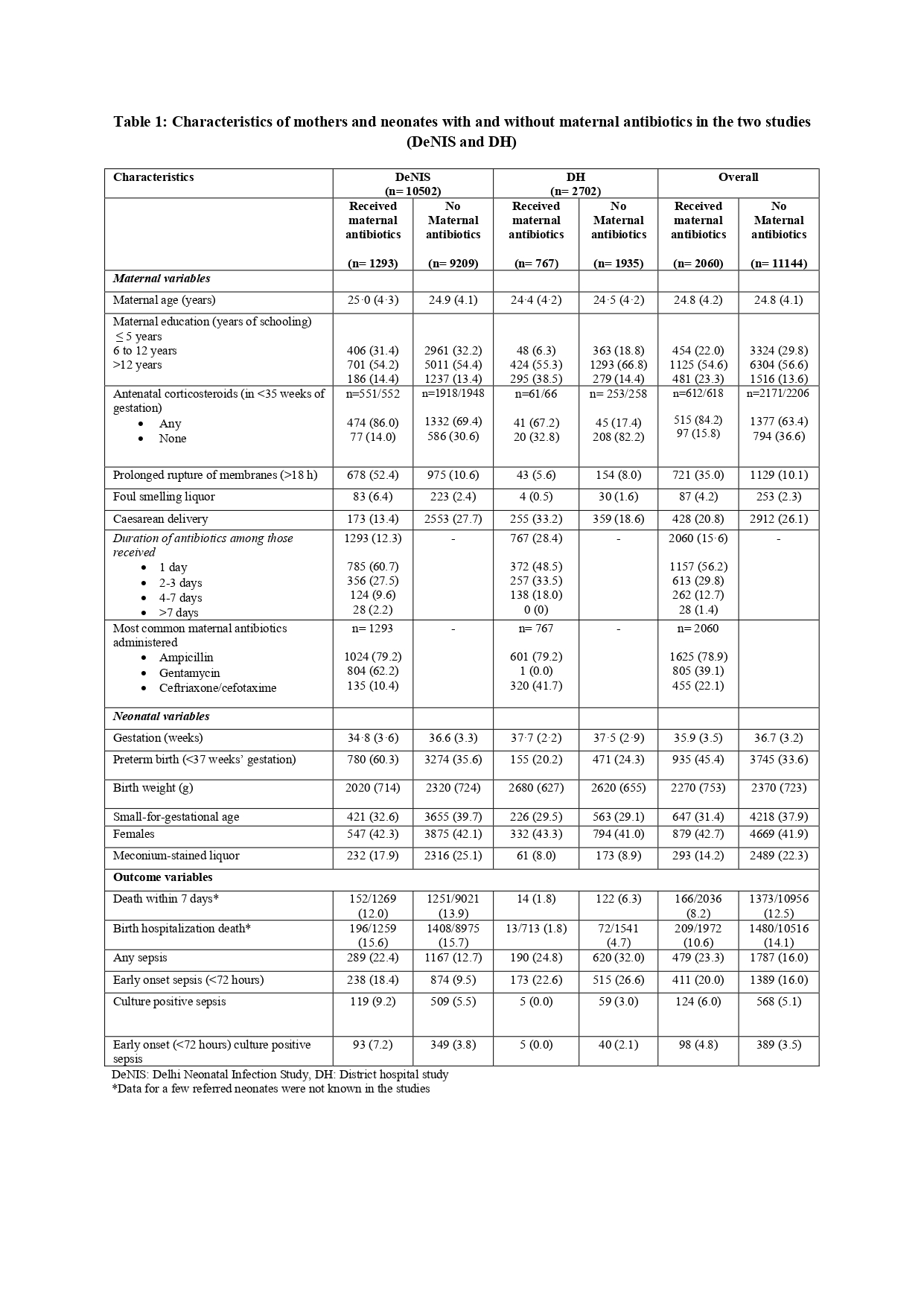 DeNIS: Delhi Neonatal Infection Study, DH: District hospital study
DeNIS: Delhi Neonatal Infection Study, DH: District hospital study*Data for a few referred neonates were not known in the studies
Table 2: Outcomes of neonates with and without maternal antibiotics in the propensity-matched cohort
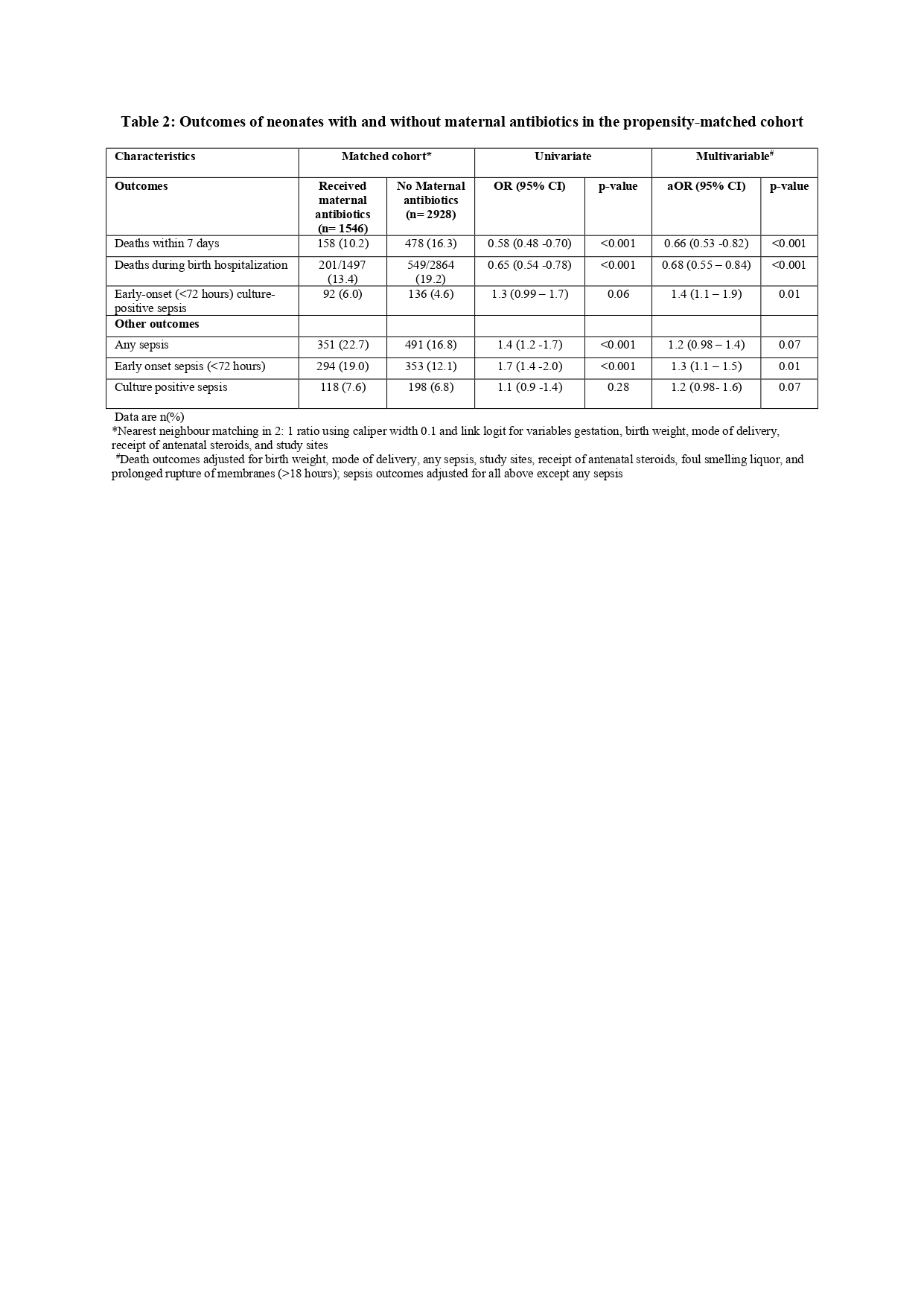 Data are n(%)
Data are n(%) *Nearest neighbour matching in 2: 1 ratio using caliper width 0.1 and link logit for variables gestation, birth weight, mode of delivery, receipt of antenatal steroids, and study sites
#Death outcomes adjusted for birth weight, mode of delivery, any sepsis, study sites, receipt of antenatal steroids, foul smelling liquor, and prolonged rupture of membranes (>18 hours); sepsis outcomes adjusted for all above except any sepsis

