Neonatal General 2: Neurology
Session: Neonatal General 2: Neurology
312 - Factors Associated with Timing of Onset of Therapeutic Hypothermia Between Inborn and Outborn Infants with Hypoxic-Ischemic Encephalopathy (HIE)
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 312.4943
Trisha Mulamreddy, University of California Davis Children's Hospital, Sacramento, CA, United States; Deepika Sankaran, University of California Davis Children's Hospital, Sacramento, CA, United States; Evan M. Giusto, UC Davis Health, Sacramento, CA, United States; Satyan Lakshminrusimha, UC Davis, Sacramento, CA, United States

Trisha Mulamreddy, MD/MPH
Resident
University of California Davis Children's Hospital
Sacramento, California, United States
Presenting Author(s)
Background: Hypoxic ischemic encephalopathy (HIE) is an important cause of neonatal morbidity and mortality. Initiation of therapeutic hypothermia (TH) within 6 hours after perinatal asphyxial insult reduces death and disability. However, there are limited data regarding barriers to timely initiation of TH and outcomes based on inborn vs outborn status.
Objective: The objective was to identify and compare factors influencing the timely initiation of TH for HIE between inborn and outborn populations.
Design/Methods: We performed a retrospective chart review of infants with HIE treated with TH between 2018-2022 at UC Davis Children’s Hospital (UCD). Data collected include place of birth (inborn vs outborn), distance of referring hospital from a level 4 neonatal intensive care unit, SARNAT scoring for neurological examination, gestational age, maternal history and complications, resuscitation at birth, Apgar scores, transport mode, transport duration, presence and timing of seizures and findings on MRI.
Results: 123 infants received TH out of which 30 were inborn and 93 were outborn during the study period (Table 1). Time of initiation of TH was shorter in inborn infants compared to outborn infants [2.3 (1.6) h vs. 5.1 (2.0) h (p < 0.001)]. More outborn infants received TH greater than 6 hours after birth (p < 0.01). Cesarean sections were more prevalent in the outborn group (p < 0.05). The duration of transport and distance of referring hospital were different among Fixed Wing, Rotor Wing, and Ground Transport for outborn infants (Table 2). Timing of initiation of TH and SARNAT Severity were not associated with transport time or distance of referring hospital from UCD (Figure 1 and 2). Incidence of seizures, MRI findings and mortality were not different.
Conclusion(s): Inborn infants received TH earlier than outborn infants and outborn infants had a higher rate of delayed TH with higher rates of cesarean deliveries. There was no difference in mortality or severity of HIE on MRI findings. Further studies are needed to investigate additional factors that influence timing of initiation of TH, use of active cooling measures during transport and its impact on outcomes.
Table 1
.png) Comparison of pregnancy, delivery and neonatal outcomes between inborn and outborn infants with HIE treated with TH
Comparison of pregnancy, delivery and neonatal outcomes between inborn and outborn infants with HIE treated with THTable 2
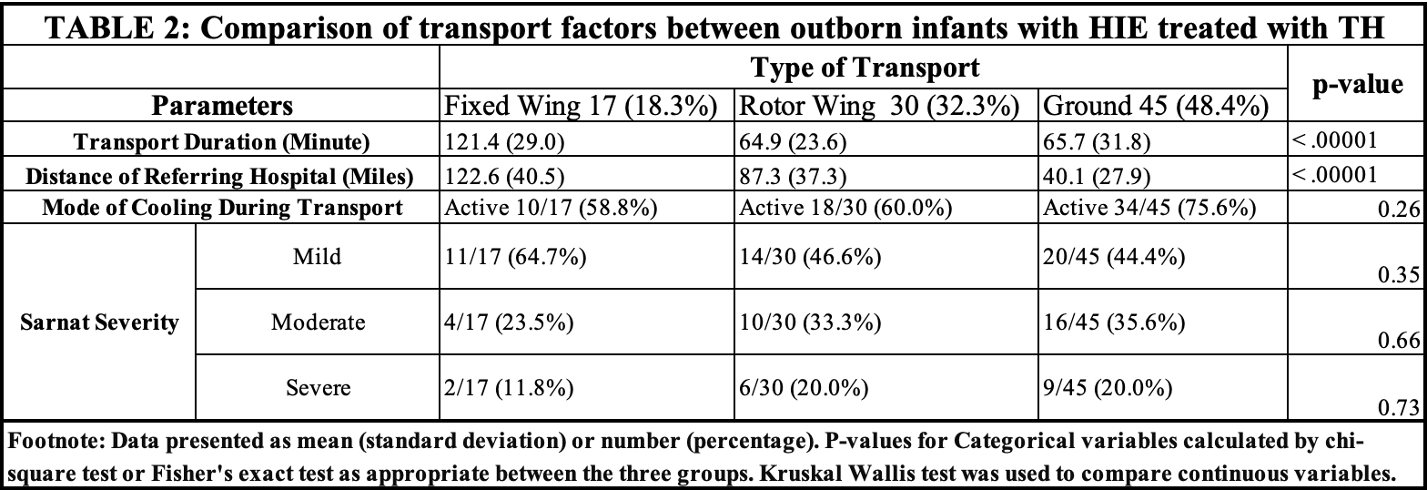 Comparison of transport factors between outborn infants with HIE treated with TH
Comparison of transport factors between outborn infants with HIE treated with THFigure 1 and Figure 2
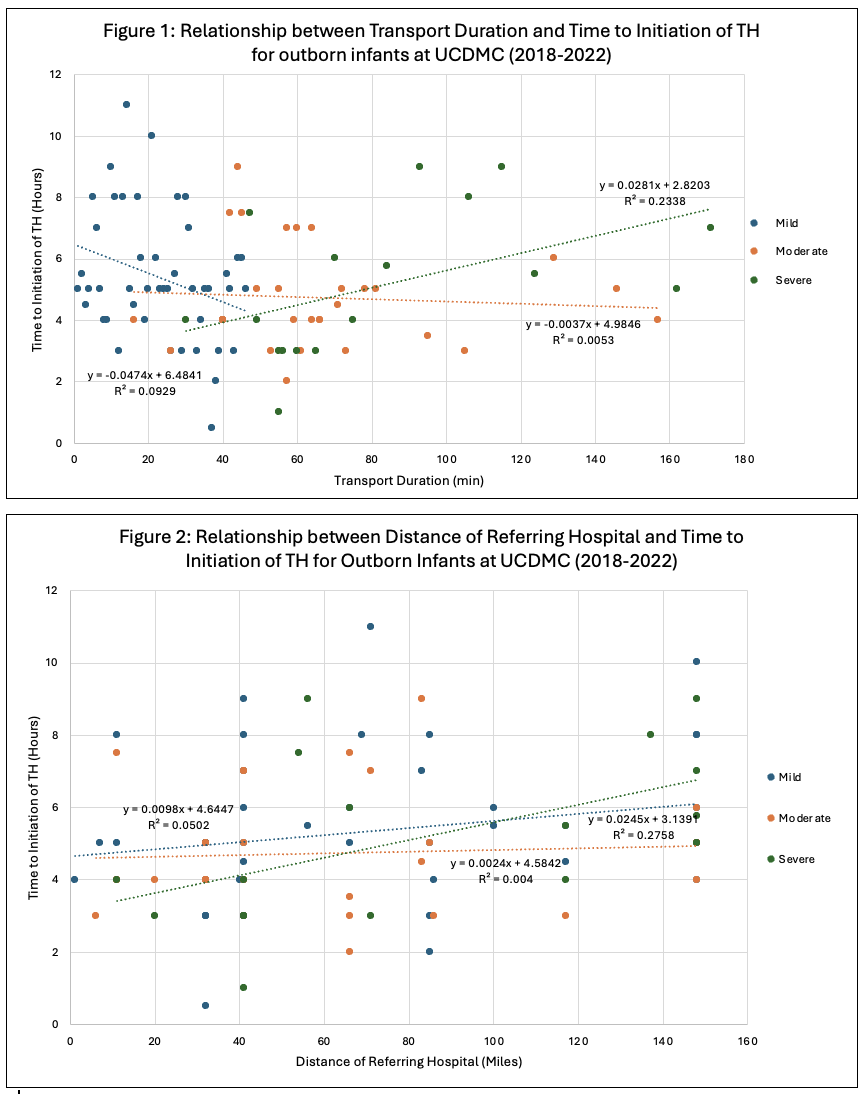 Relationship between transport duration, Sarnat severity, and distance of referring hospital with timing of initiation of TH for outborn infants with HIE.
Relationship between transport duration, Sarnat severity, and distance of referring hospital with timing of initiation of TH for outborn infants with HIE.
