Neonatal Neurology 3
Session: Neonatal Neurology 3
362 - Combining 47 clinical and neuroimaging variables to predict adverse 18-22-month outcomes for Hypoxic Ischemic Encephalopathy in Neonatal Research Network trials
Friday, April 25, 2025
5:30pm - 7:45pm HST
Publication Number: 362.4550
Yangming Ou, Boston Children's Hospital, Boston, MA, United States; Ankush Kesri, Boston Children's Hospital, Boston, MA, United States; rina bao, Boston Children's Hospital, Boston, MA, United States; Chuan-Heng Hsiao, Boston Children's Hospital, Brookline, MA, United States; Rutvi Vyas, Boston Children's Hospital, Boston, MA, United States; Mohammad Arafat Hussain, Boston Children's Hospital/Harvard Medical School, Quincy, MA, United States; Scott A.. McDonald, RTI International, Raleigh, NC, United States; Jeanette O. Auman, RTI, Durham, NC, United States; Anna N.. Foster, Boston Children's Hospital, Boston, MA, United States; Janet Soul, Boston Children's Hospital, Boston, MA, United States; Erfan Darzidehkalani, Boston Childrens hospital, Boston, MA, United States; Matheus Dorigatti Soldatelli, Boston Children's Hospital, Boston, MA, United States; Seetha Shankaran, The University of Texas at Austin, Ann Arbor, MI, United States; Abbot Laptook, Women & Infants Hospital of Rhode Island, Providence, RI, United States; Michael Cotten, Duke university, Durham, NC, United States; Patricia Ellen. Grant, Boston Children's Hospital, Boston, MA, United States
- YO
Yangming Ou, PhD
Associate Professor
Boston Children's Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Hypoxic ischemic encephalopathy (HIE) affects in 1~5/1000 term infants. Despite treatment, 1/3 of neonates with HIE shown adverse outcomes by age 2 years. The Consortium Of Biomarker In Neonatal Encephalopathy (COMBINE, since 2022), aims to predict 2-year adverse outcomes in the neonatal stage, toward improving care in early time windows. We merged 2 HIE trials - Late Hypothermia (2008-16, late/standard cooling or control arms, 21 sites) [1] and Optimizing Cooling (2010-14, standard/longer/deeper cooling arms, 18 sites) [2].
Objective: Develop a multivariate machine learning predictor and quantify the accuracy in predicting 18-22-month adverse outcomes.
Design/Methods: We started from 47 variables based on clinical knowledge (Table 1). Experts scored severity of brain injury in neonatal brain MRI, using the Neonatal Research Network (NRN) scoring system: 0 no injury, 1a, 1b, 2a, 2b, and 3 devastating injuries [3]. Outcome was adverse (N=312, moderate/severe disability, or death), or normal (N=95) by 18-22 months. Our algorithm automatically selected the subset of variables with the highest prediction accuracy compared to other variable combinations, by a consensus of linear support vector machine, gaussian SVM and random forest. Accuracy was defined as percentage of neonates being predicted correctly, in 5-fold cross validation (80% patients training; 20% patients testing; repeated 5 times so every patient has been tested once and only once).
Results: Expert NRN score of neonatal brain MRI alone achieved 0.84 accuracy. When NRN score of MRI was not used, machine learning selected 12 out of 46 clinical variables for a 0.84 accuracy. The highest accuracy, 0.89, was obtained by combining NRN expert score and clinical variables. Of the 9 variables finally selected to predict outcomes, the most predictive variables were NRN expert score of MRI, treatment variables (Sarnat scores at discharge and post-treatment, intubation), neonatal characteristics (1min Apgar, gestational age), maternal demographics (age, race), and delivery mode. In contrast, [4] found 0.85 accuracy predicting motor impairment at 1-2 years in 117 infants, combining MRI injury in putamen/globus pallidus, gestational age, and umbilical cord pH.
Conclusion(s): Expert NRN score of neonatal brain MRI, treatment, neonatal characteristics, maternal demographics, and delivery mode jointly predicted 18-22-month adverse outcomes with 0.89 accuracy. Future work will add more sophisticated MRI analysis, more comprehensive clinical variables, and more tests of accuracy stability across multi-site data.
Table 1
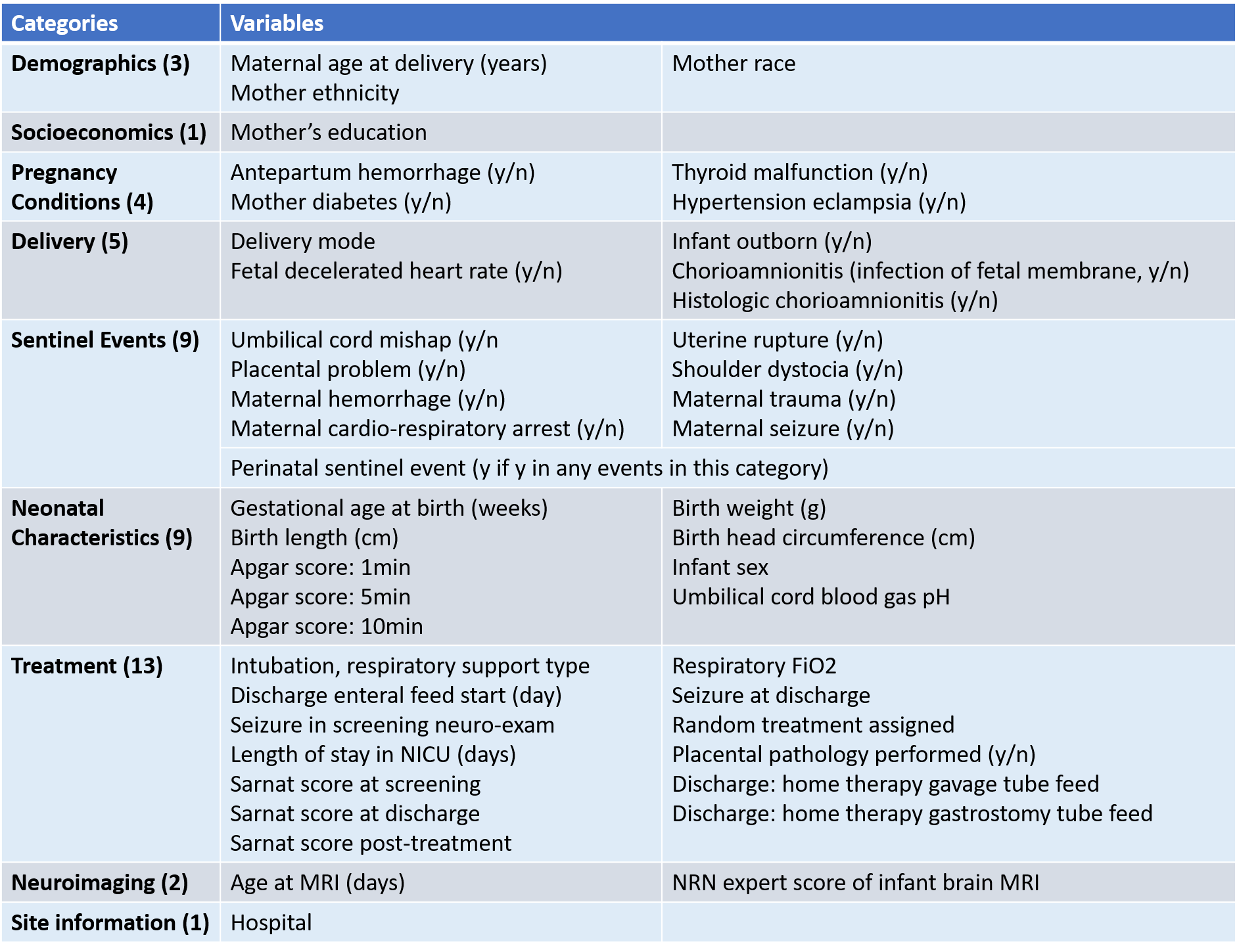 Table 1. The 47 clinical and MRI variables we have included as predictors in this study.
Table 1. The 47 clinical and MRI variables we have included as predictors in this study. Fig 1
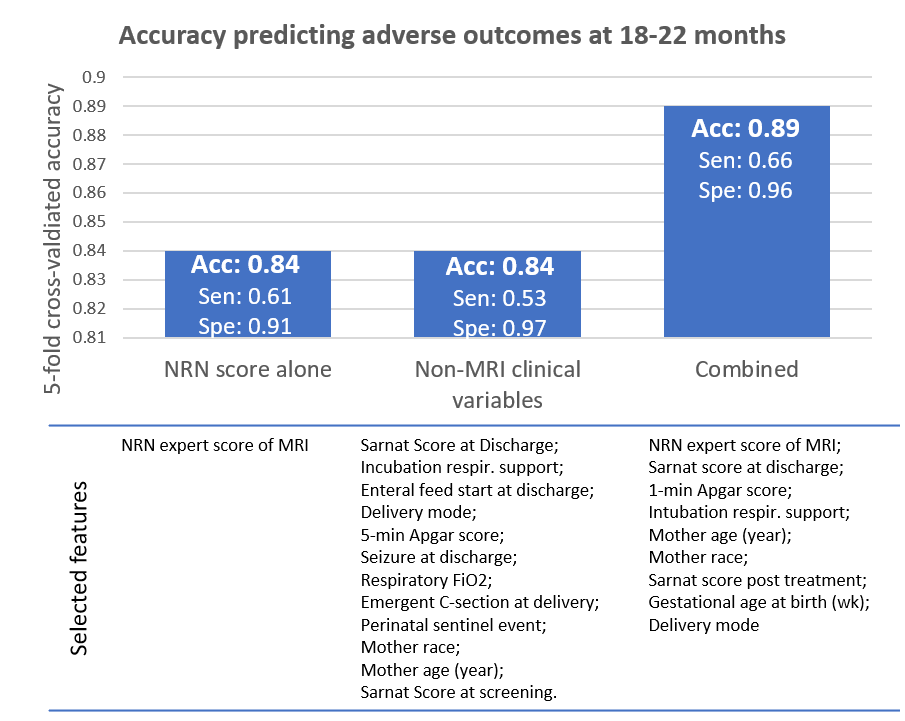 Fig 1. Accuracies and auto-selected variables in three experiments for outcome prediction.
Fig 1. Accuracies and auto-selected variables in three experiments for outcome prediction.
